Clinical:
- A 64 years old man
- Underlying HPT, DM and old CVA
- Complaint sudden onset giddiness, vomiting and nausea, tinnitus, unsteady gait with tendency to fall to left side.
- Clinically: no neurological deficits, no cerebellar sign/nystagmus
- CT scan was normal
MRI findings:
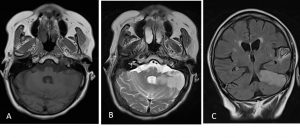
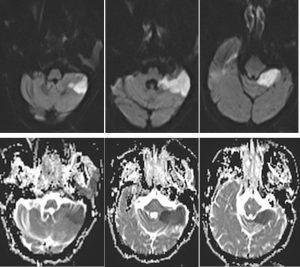
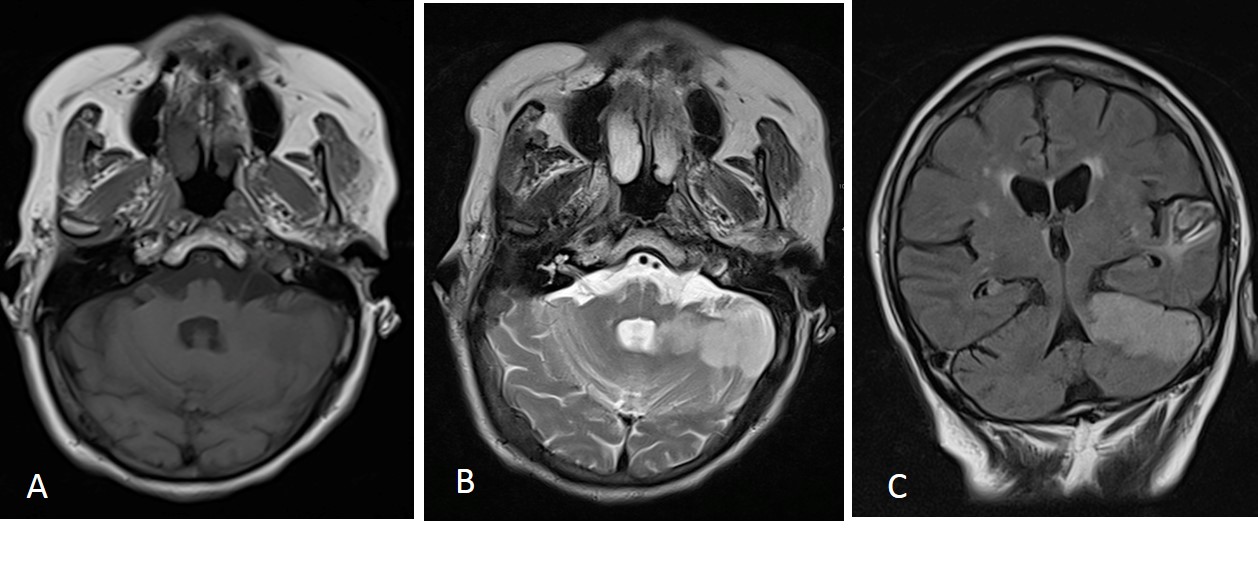
- There is a large wedge shaped area of abnormal signal involving both grey and white matter of superior left cerebellar hemisphere.
- It is hypointense to surrounding grey matter on T1WI, hyperintense on T2WI and FLAIR, demonstrates diffusion restriction, and is associated with effacement of adjacent sulci.
- No compression of adjacent 4th ventricle.
- No blooming artefact on GRE to suggest haemorrhage within
Diagnosis: Acute infarction of left superior cebellar territory.
Discussion:
- Superior cerebellar artery arises near the termination of the basilar artery
- It supplies superior part of the cerebellum, cerebellar vermis and part of the midbrain
- Imaging features of stroke involve these regions
- Occlusion at the origin of the artery produces the classic presentation of ipsilateral cerebellar (ataxia, dysarthria, nystagmus) and brainstem (Horner’s syndrome) signs associated with a contralateral dissociated sensory impairment.
- Peripheral occlusion presents with solely ipsilateral cerebellar signs
Recent Comments