Case contribution: Dr Radhiana Hassan
Clinical:
- A 52 years old man with underlying DM and hypertension
- Presented with severe headache for few days
- Initially admitted to a hospital, CT brain reported normal
- Patient took AOR despite unresolved headache
- Later he was admitted to another hospital
- Another CT scan brain done and reported normal again
- During hospitalisation, patient had one episode of seizures followed by drowsiness
- Currently GCS=E4VtM5, pupils 3+/3+, Power bilateral lower limbs are 3/5
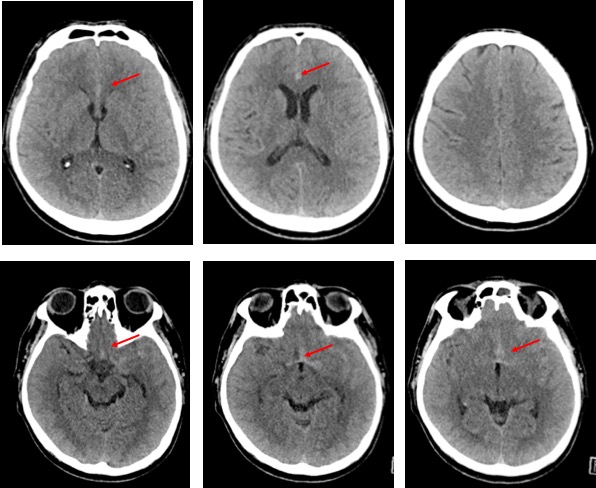
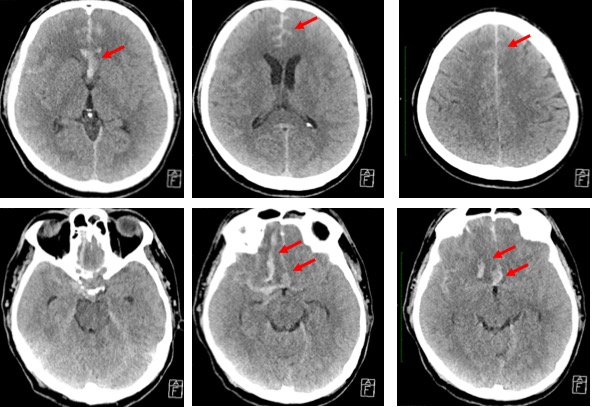
CT scan findings:
- Initial CT scan shows subtle hyperdensity in the interhemispheric region which is worse on subsequent scan
- Extension of bleed into right sylvian fissure, and in the suprasellar cistern extending to the interpeduncular cistern.
- There is also intraparenchymal hemorrhage with surrounding oedema of right frontal lobe on subsequent scan
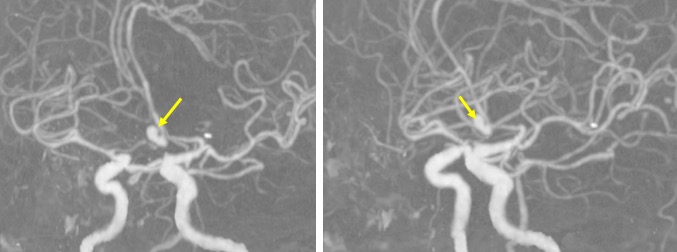
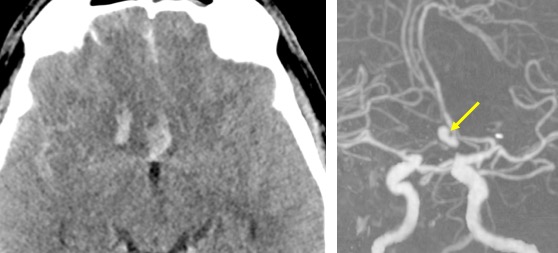
CT angiogram findings:
- A lobulated aneurysm with wide neck seen arising from the ACOM
- It is pointing anteriorly, no active contrast extravasation
Diagnosis: Ruptured ACOM aneurysm
Discussion:
- Subarachnoid hemorrhage secondary to ruptured cerebral aneurysm results in significant morbidity and mortality.
- Clinical outcomes after aneurysm rupture and treatment are influenced by cumulative cerebral infarction burden.
- Anterior communicating artery aneurysms (AcomAs) are among the most commonly identified ruptured aneurysms
- AcomA rupture and treatment are more strongly associated with cognitive and behavioral deficits relative to other aneurysm locations
- The cause of these neuropsychiatric deficits remains uncertain, but prior studies have suggested ischemic injury to the frontal cortex, ventromedial prefrontal (orbitofrontal) cortex, or striatum as a possible etiology.
Recent Comments