Case contribution: Dr Radhiana Hassan
Clinical:
- A 2 years old female, previously healthy with no underlying medical problem
- Alleged fall from sofa 3 months ago, frontal head hit the floor. Post fall patient was well and active as usual
- Noted by mother a swelling at head for last one week. No fever, no vomiting. Otherwise child was active and feeding well.
- Clinical examination in ED shows child active. Dysmorphic features (forehead is larger than normal), sunset eyes, no nystagmus. Two swelling at right parietal region, non tender, no skin changes. Both upper and lower limbs show no neurological deficit.
- CT scan requested for post traumatic hydrocephalus.
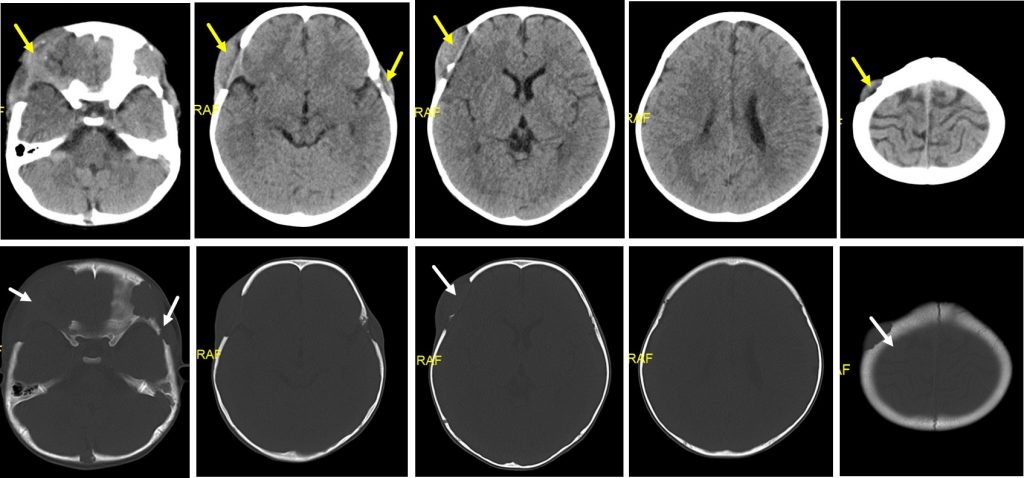
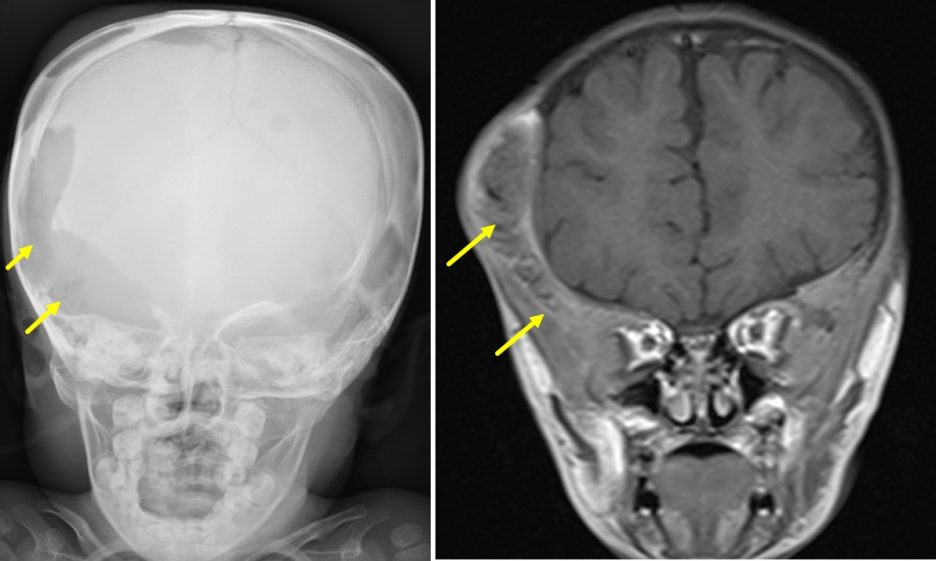
CT scan findings:
- There are multiple osteolytic bone lesions (white arrows) with soft tissue component (yellow arrows) involving skull vault
- The largest is seen at right frontotemporal region measuring about 2.0 x 5.3 x 5.5 cm (AP x W x CC).
- However no intracranial extension.
- No acute intracranial haemorrhage. No focal brain parenchymal lesion.
- Ventricles and CSF spaces are unremarkable.
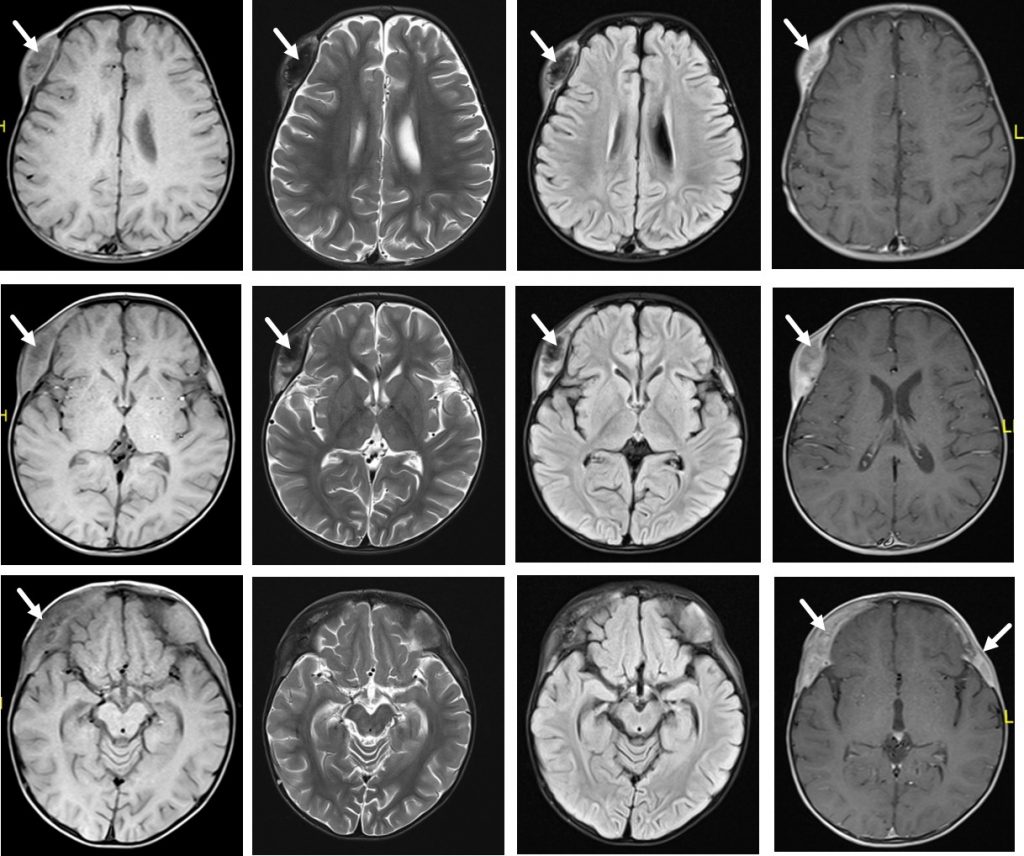
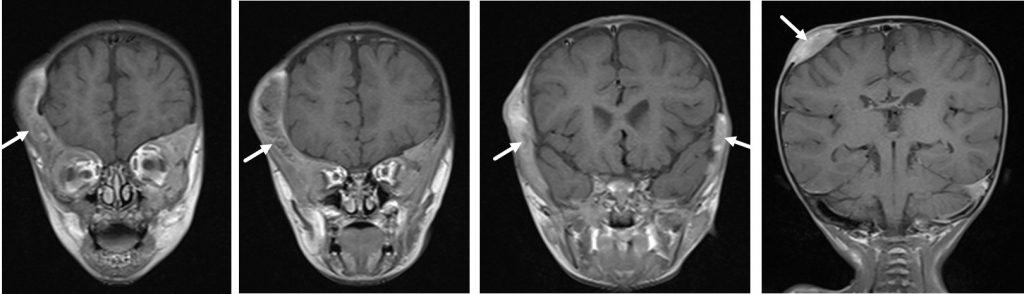
MRI findings:
- The lesion at right frontotemporal region infiltrates the outer table, the diploic space and erodes the inner table involving overlying fronto-temporal bone, supraorbital roof of right frontal bone, right greater wing of sphenoid and right zygomatic bone.
- This lesion appears to extend into the lateral extraconal fat of right intraorbital space abutting the superior rectus muscle. The rest of the extraocular muscles and intraconal fat pads are normal.
- Another lesion left frontotemporal region involving left frontal bone, lateral wall of left orbital, left temporal bone and left zygomatic bone. This lesion is also extending into the lateral extraconal fat of left intraorbital space. However the left extraocular muscles and intraconal fat pads are intact. No displacement of the orbit is seen.
- Similar lesions are also seen at the right parietal region. There are multiple bone erosions are seen left temporal bone, left frontal bone, right occipital bone, right greater wing of sphenoid, left greater wing of sphenoid, clivus, left occipital condyle and left mastoid cells.
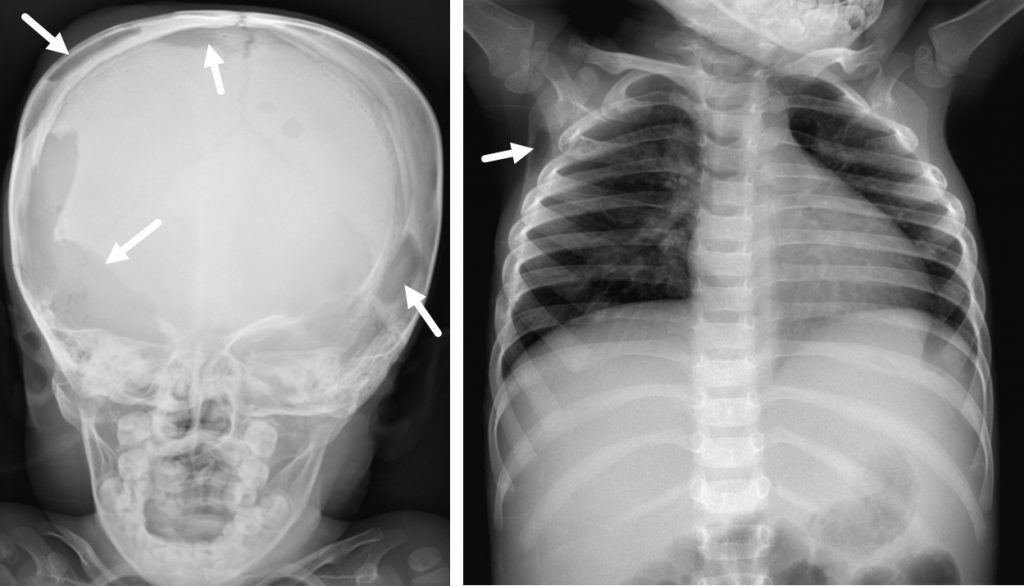
Skeletal survey shows lytic changes at multiple sites of the bones.
HPE findings:
- Macroscopy: lesion labelled as scalp lesion, consists of multiple pieces of tan-whitish tissue measuring 7 mm in aggregate diameter.
- Microscopy: Sections show multiple fragments of fibrocollagenous tissue and tumour tissue. The tumour is composed of numerous histiocytic Langerhans cells displaying irregular nuclei with nuclear indentation and grooving, fine chromatin, inconspiciousto small nucleoli, and ample cytoplasm. No obvious atypia or pleomorphism noted. The background shows reactive cellular infiltrates comprising eosinophils, neutrophils, histiocytes, lymphocytes and plasma cells. Multinucleated cells are also present. Foci or necrosis are observed.
- Immunohistochemistry: The Langerhans cells are positive for S100, CD68 and CD1a.
- Interpretation: Scalp lesion consistent with Langerhans cell histiocystosis
Diagnosis: Langerhans cell histiocytosis (LCH)
Discussion:
- LCH is more common in the paediatric population with a peak incidence between one and three years of age.
- Incidence is estimated at ~5 per million children, and 1-2 cases per million adults 8. There is also a slight male predilection.
- Any part of the body can be affected and clinical presentation depends on specific involvement.
- The course of the disease ranges from those that spontaneously regress to those that have a rapidly progressive course.