Case contribution: Dr Radhiana Hassan
Clinical:
- A 29-years old male
- Underlying neurofibromatosis 1
- Presented at 6 years of age with multiple cutaneous nodule
- Presented with increase in size of one of the nodules at left calf in 6 months, associated with pain
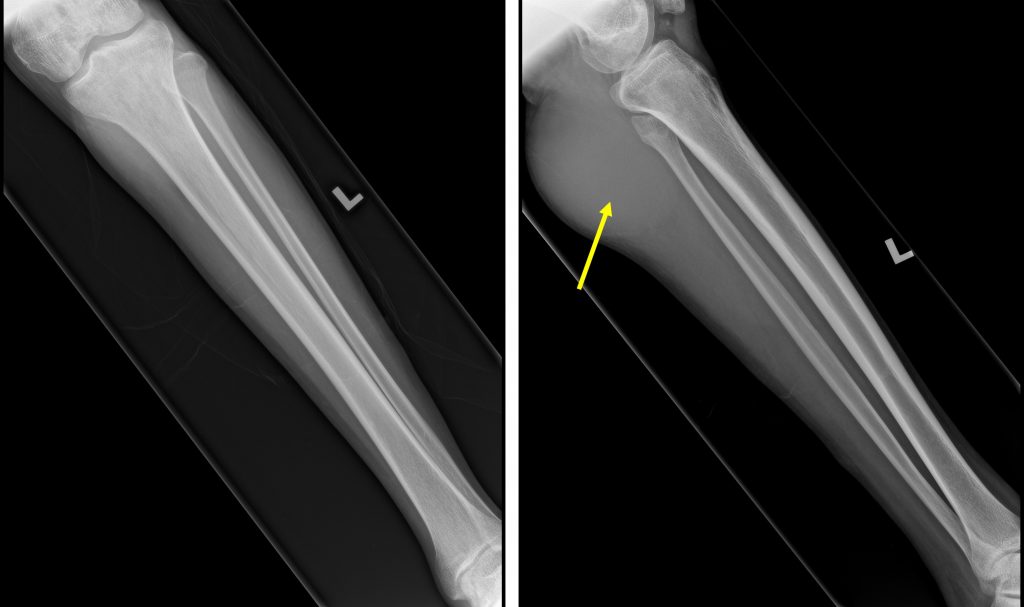
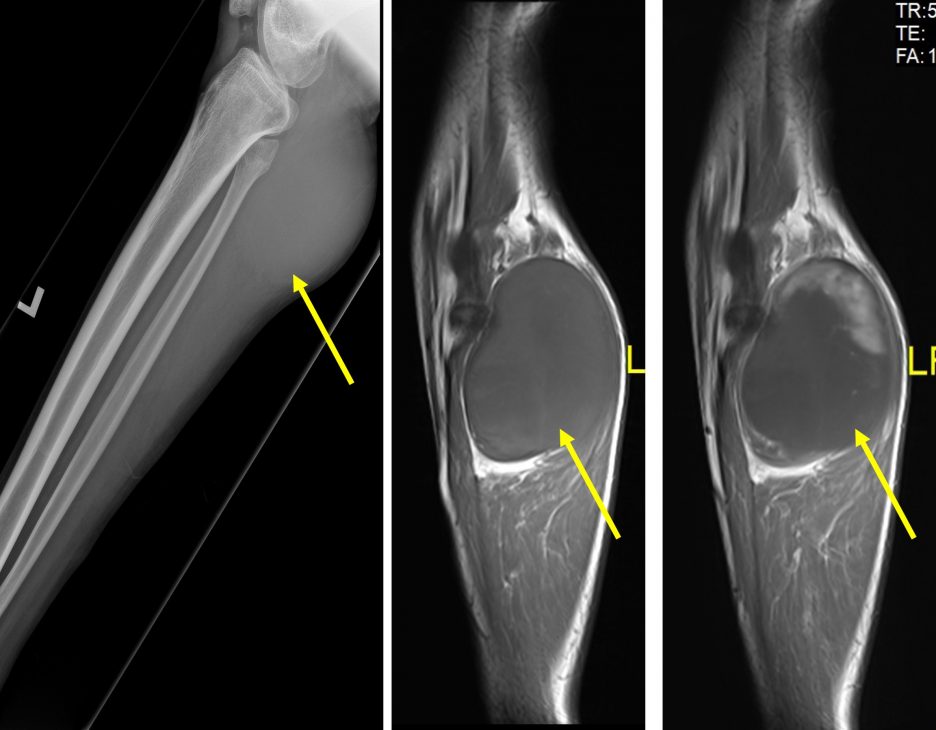
Radiograph of left leg in AP and lateral views:
- There is soft tissue swelling seen at posterior aspect of proximal tibia fibula (yellow arrow).
- No calcification or air pocket seen within the swelling.
- The visualised bones are unremarkable. No lytic or sclerotic lesion. No bony erosion.
- Visualised knee and ankle joints are unremarkable.
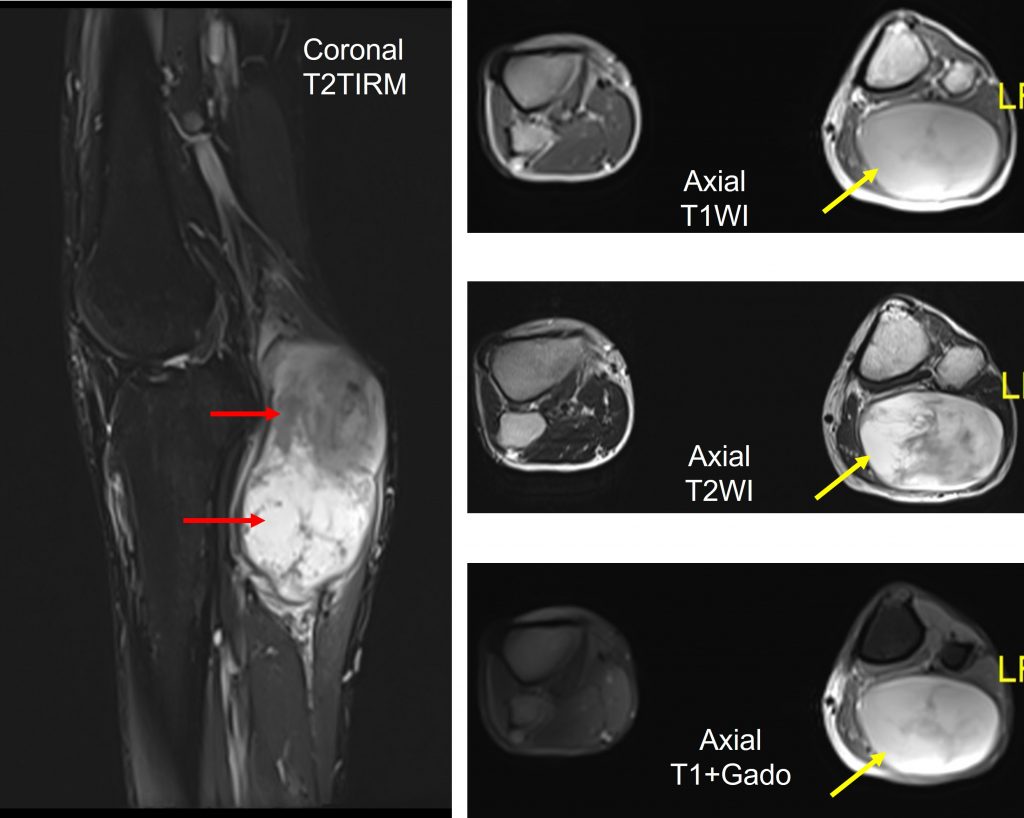
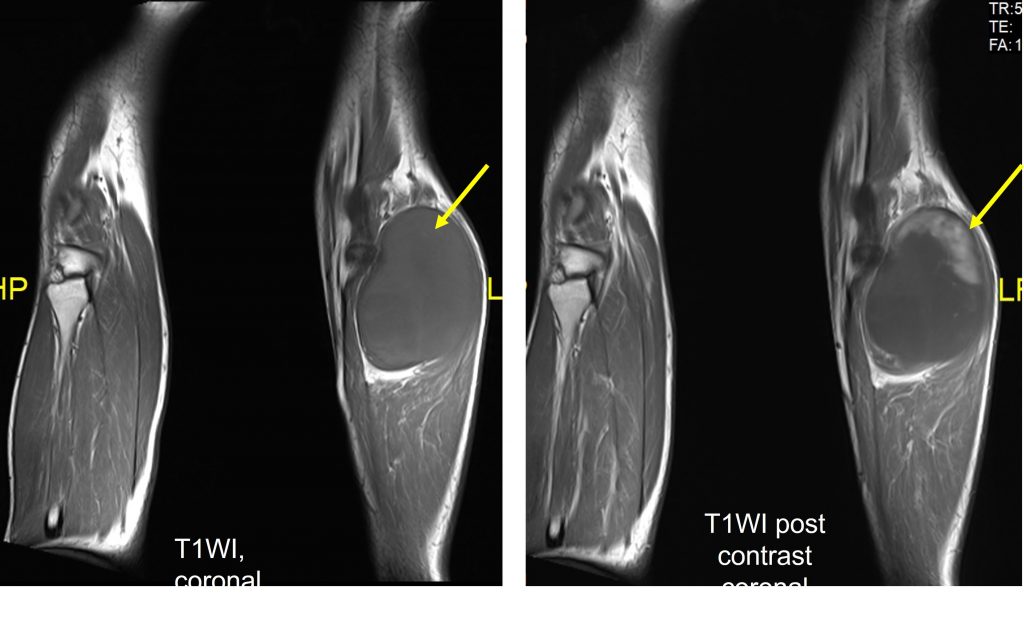
MRI of lower limb:
- There is a well-circumscribed encapsulated oval-shaped mass seen at the posterior compartment of proximal left calf region, measuring approximately 5.7 x 8.3 x 10.9 cm (AP x W x CC).
- It appears isointense to muscle on T1W and heterogeneous hyperintense on T2W. In post contrast study, heterogeneous enhancement is seen at the periphery of superior aspect of the mass.
- The mass is also causing mass effect to the adjacent muscles and splaying the gastrocnemius and popliteus muscles however clear plane of demarcation are still seen in between. No intramuscular extension, infiltration or muscle oedema.
- No cortical destruction of the adjacent bones. No focal bone lesion or marrow oedema is observed.
- No adjacent subcutaneous fat streakiness or skin break. Knee joint is preserved.
Tru-cut biopsy of mass lesion:
- Macroscopy:Received a specimen labelled as soft tissue tumour posterior left calf consists of 2 strips of whitish tissue measuring 10-11 mm in length.
- Microscopy:Section shows strips of tumour tissue composed of spindle cells proliferation in a background of collagenous and myxoid stroma. The spindle cells predominantly bland spindle cells with thin and wavy nuclei. In areas, mild nuclear atypia is noted exhibiting enlarged nuclei with hyperchromatism. No mitosis or necrosis seen.
- Impression: spindle cell neoplasm with neural differentiation favours neurofibroma.
Excision of mass done:
- Macroscopy: Sections from the tumour shows a fairly circumscribed tumour composed of alternating hypocellular and hypercellular area. The tumours are arranged in fascicles with a hemangiopericytoma-like vascular pattern. The tumour cells at hypercellular area display moderate to marked pleomorphic nuclei, hyperchromatic to vesicular nuclei with prominent nucleoli. Scattered multinucleated tumour giant cells are noted. Mitoses are easily seen, including abnormal form. Large areas of necrosis are present. The tumour cells at hypocellular are shows uniform spindle cells with hyperchromatic, thin and wavy nuclei. The stroma are fibromyxoid. NO lymphovascular invasion noted. No heterologous differentiation identified. The skeletal muscle and skin are free from malignant cell infiltration.
- Microscopy: Specimen labelled as neurofibroma cosists of an ellipse of skin measuring 45x16x2 mm with underlying encapsulated tumour measuring 110x80x80 mm and adjacent fatty tissue and skeletal muscle measuroing 20x40x10mm. Cut section shows a well-circumscribed greyish tumour with tan greyish surface and multiple small cystic spaces. No hemorrhage or necrosis seen. Grossly the tumour is located 1 mm from proximal margin, 1 mm from distal margin, 1 mm from lateral margin 1 mm from anterior and posterior margin. The overlying skin is unremarkable.
- Impression: Malignant peripheral nerve sheath tumour, high grade TNM stage pTNM, AJCC
Diagnosis: Malignant Peripheral Nerve Sheath Tumour
Discussion:
- Occur either de novo or arising from pre existing tumour such as neurofibromas or schwannomas etc
- About half of such tumours are seen in individuals with neurofibromatosis type 1 (NF1)
- Typically present in young and middle aged adult, no gender predilection
- These tumours are often fairly rapid enlarging and clinical presentation depends on site of tumour
- Aggressive tumour that carry a poor prognosis. Overall 5-year survival rate for sporadic tumour is 65%.
- Poor prognostic factor include: NF-1, large size, location at the trunk and high grade histological features
Recent Comments