Case contribution: Dr Radhiana Hassan
Clinical:
- A 53 years old man
- presented with difficulty in speech and memory loss
- Gradual onset and worsening, disorientated at times
- No headache, no seizure, no blurring of vision
- No fever, no trauma
- HIV antigen and antibody -ve
- Work out for TB all negative
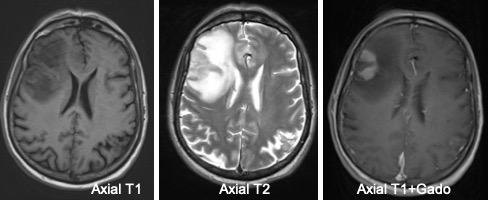
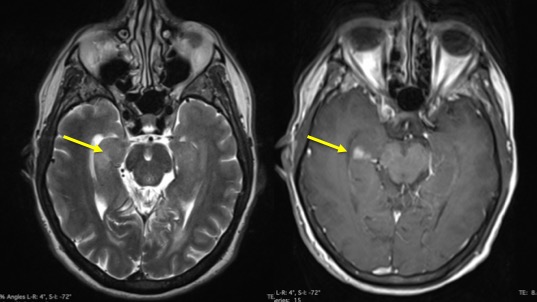

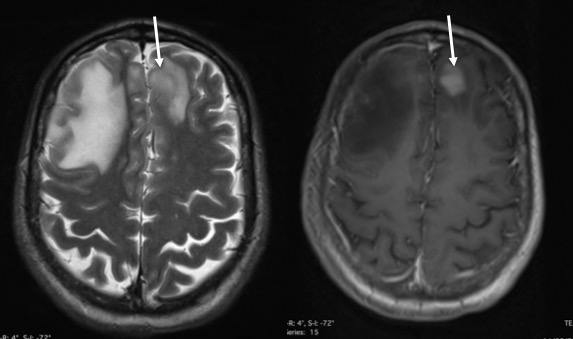
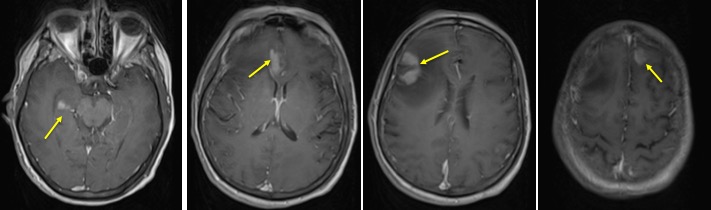
MRI findings:
- There are multiple ill-defined lesions, largest at right frontal region.
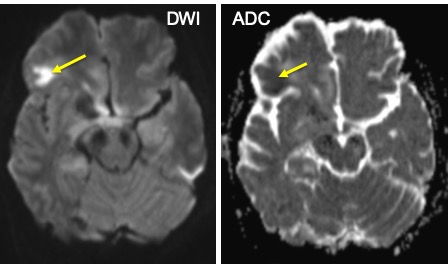
- The enhancing part showed restricted diffusion on DWI/ADC
- The lesions are predominantly hyperintense on T1, isointense on T2 and enhanced post gadolinium
- No blooming artifact on SWI (images not shown)
- There is marked perilesional oedema
- Other lesions are smaller at parasagittal of right frontal, left frontal, corpus callosum and right temporal
- No hydrocephalus
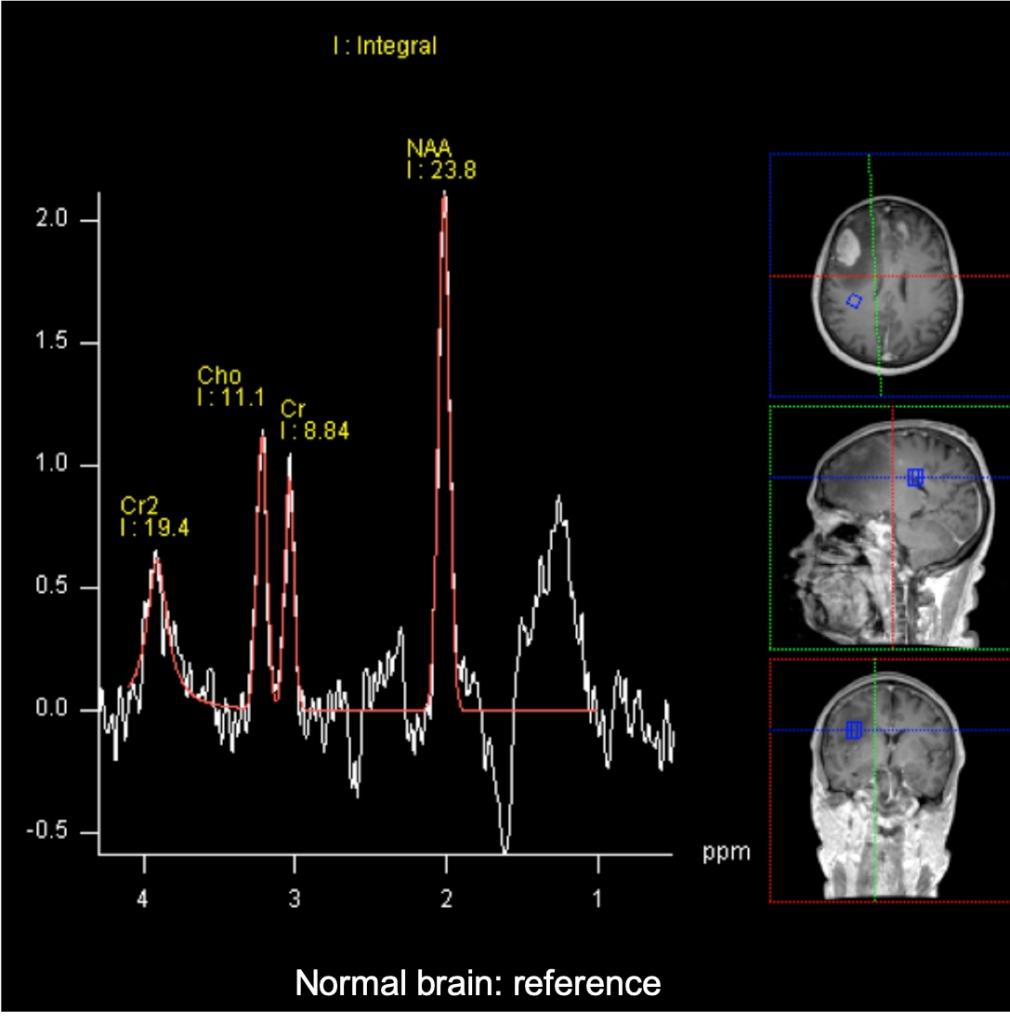
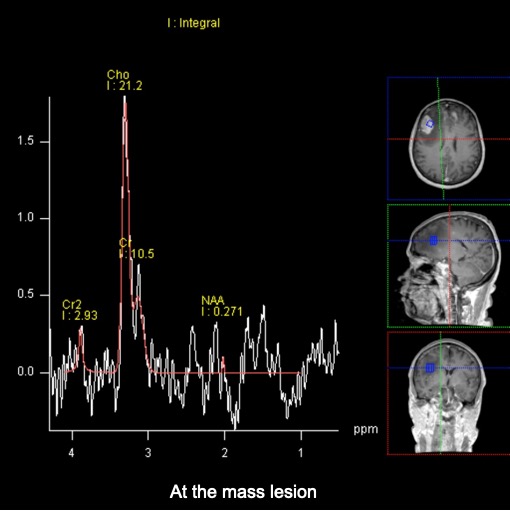
- MR spectrospcy showed significant choline/NAA reversal (images below)
Histopathological result:
- Macroscopic: Specimen labeled as soft tumor (superficial) and hard tumour (deep) composed of multiple fragments of whitish tissue measuring 25 mm in aggregate diameter.
- Microscopic: Section shows multiple fragments of brain tissue diffusely infiltrated by atypical lymphoid cells which are predominantly forming perivascular cuffs. The lymphoid cells are medium to large in size and display hyperchromatic nuclei, occasional conspicuous nucleoli and scanty cytoplasm. Many mitosis and apoptotic bodies are also observed.
- Immunohistochemical studies show the atypical lymphoid cells are positive for CD20, BCL2 & MUM1, scatteredly positive to BCL6 and negative to CD3. The proliferative index is high (80%). Synaptophysin highlights the neuronal background of the brain tissue.
- GFAP staining shows presence of reactive astrocytic cells.
Diagnosis: Brain tumor: Diffuse large B-cell lymphoma
Progress of patient:
- BMA and Trephine biopsy showed no blast cells
- US testes showed no testicular lesion
- CT Thorax, abdomen and pelvis are unremarkable
Primary CNS lymphoma:
- Extranodal malignant lymphoma arising in CNS in absence of systemic lymphoma
- In immunocompetent patient, 6th to 7th decade
- In immunocompromised patient mean age of 39 years
- Gender: male predominance
- Location: 60-80% are supratentorial, deep gray nuclei commonly affected, often involve and cross corpus callosum, frequently abut and extend along the ependymal surfaces
- Morphology: can be solitary mass or multiple lesions
- Imaging and prognosis varies with immune status
- Periventricular and subependymal involvement is characteristic
- NECT: classically hyperdense, may be isodense, may or may not contain hemorrhage/necrosis
- CECT: commonly show moderate and uniform enhancement, can be ring-enhancement in immunocompromised patient
- MRI: may be heterogenous signal from hemorrhage and necrosis, may show restricted diffusion, strong homogenous enhancement post contrast, MRS with low NAA and high CHo
- Steroid may dramatically reduced the mass, reduced the enhancement and mask biopsy result