Clinical
- A 22 years old man
- Presented with sudden onset of generalized tonic clonic fit. He had no history of childhood seizure.
- He had localized headaches and a skull swelling noted few months before the fitting episode.
- No loss of appetite or loss of weight
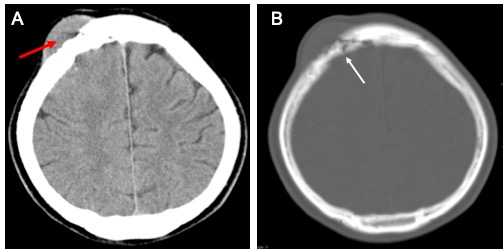
CT findings:
- There is a destructive lytic lesion of the right frontal bone (white arrow) with surrounding soft tissue swelling (red arrow).
- Small foci of calcification seen in the adjacent brain parenchyma.
- Associated subtle effacement of adjacent brain parenchyma
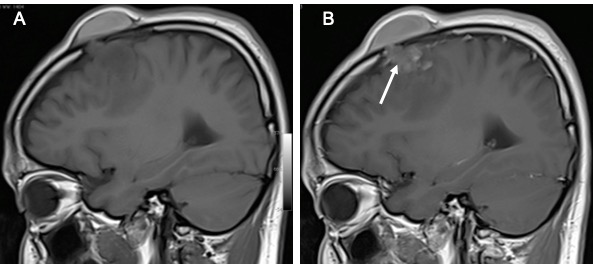
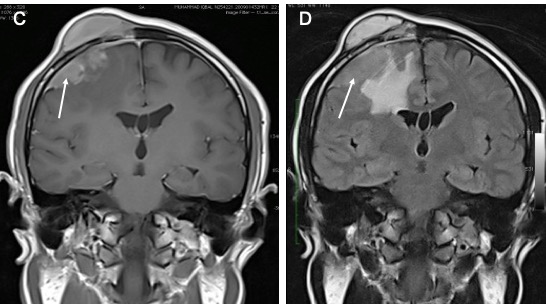
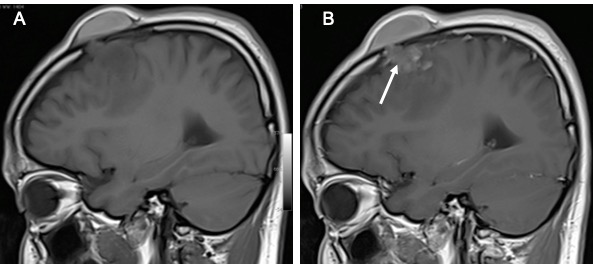
MRI findings:
- A lobulated broad-based lesion at right frontal lobe (white arrows)
- It is isointense on T1, slightly hyperintense on T2 and homgenously enhances post contrast
- Dural tail seen
- No central necrosis seen
- Associated marked perileseional oedema
- Bony and scalp infiltration as noted on CT scan
HPE findings:
- Subcutaneous tumour: highly cellular tumour cells in sheet-like pattern. Cells moderately pleomorphic.
- Brain tumours: 30 mm in aggregate diameter. Cut section shows whitish appearance. Microscopically shows highly cellular tumour cells arranged in sheet-like pattern. Tumour cells display moderate pleomorphism with large oval nucleus with central clearing and indistinct cytoplasmic borders. Some showed prominent nucleoli. Mitosis occasionally seen (1/10hpf). Tumour necrosis seen. Surrounding tissue is infiltrated by chronic inflammatory cells.
- Immunohistochemical stain shows malignant cells positive for EMA, ki-67 with proliferation index 10%.
Diagnosis: Atypical meningioma with skull infiltration, WHO Grade II.
Discussion: Atypical meningioma
- Most meningiomas are benign and classified as grade I according to World Health Organization (WHO) standards
- Atypical meningiomas account for between 4.7 and 7.2% of all meningiomas
- Malignant meningiomas are less common, comprising between 1.0 and 2.8%
- It should be noted that epidemiology, clinical presentation, and radiographic features do not reliably distinguish these different types of meningiomas.
- Generally, atypical meningiomas grow faster, have more heterogeneous/aggressive imaging appearances, and have a tendency to recur early.
- The presence of vasogenic edema in adjacent brain parenchyma is not a predictor of atypical or anaplastic histology
- The five-year recurrence rate is significantly higher (41%) than that seen in grade I (benign) meningiomas (12%)
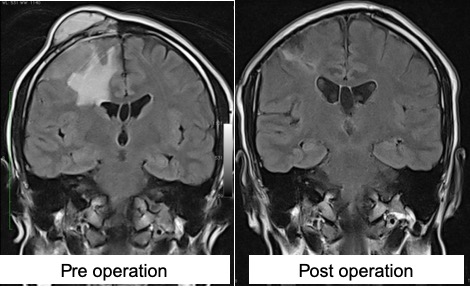
Progress of patient:
- Patient had operation done
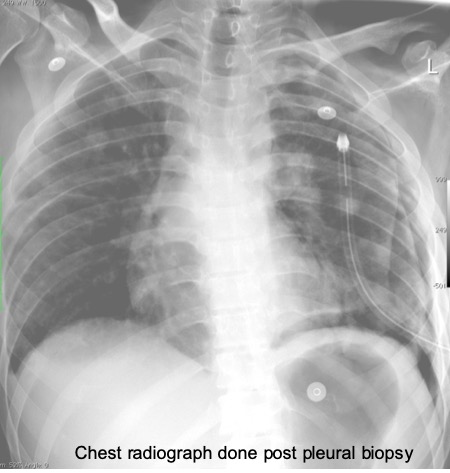
- 2 years later patient presented with acute shortness of breath and noted to have massive pleural effusion with multiple lung metastasis
- Pleural biopsy done concluded as morphological, immunohistochemical and clinical presentation are compatible with metastatic meningioma