Clinical:
- A 78-year old lady with no known medical illness
- Presented with first episode generalized tonic clonic seizure.
- No history of trauma.
- Blood pressure was normal.
- Urgent non-contrast CT scan showed acute intraparenchymal hemorrhage at high parietal region on the right side.
- MRI was performed 3 weeks later.
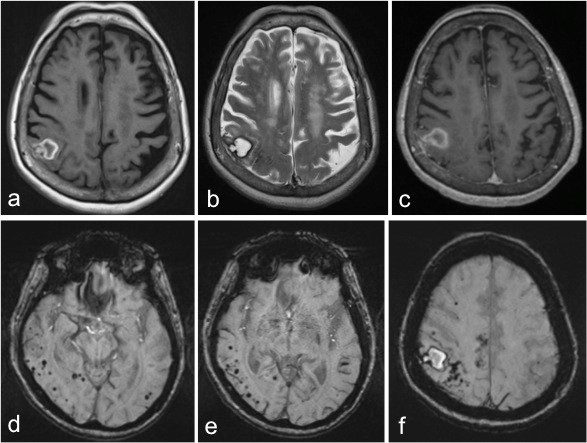
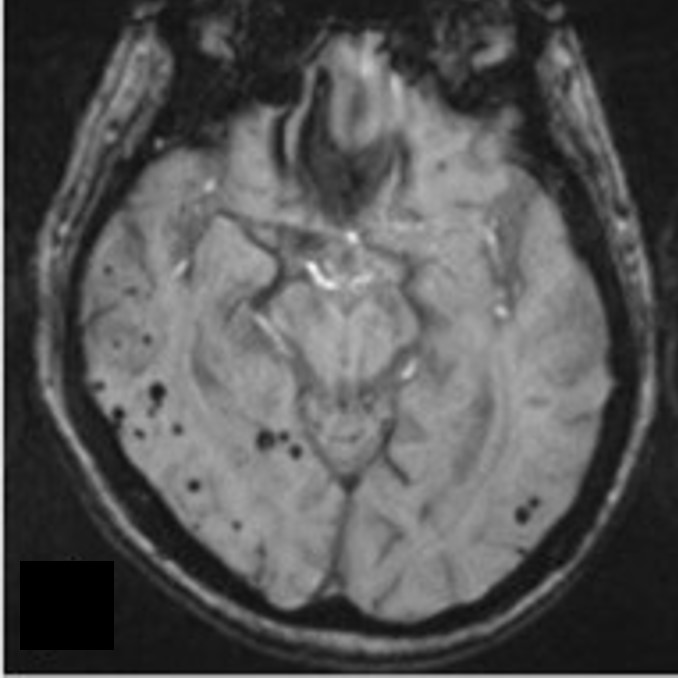
MRI findings:
- MRI of the brain in axial plane (a) T1-weighted image, (b) T2-weighted image, (c) T1-post contrast and (d-f) SWI sequence.
- A chronic right parietal parenchymal haematoma is demonstrated by low signal intensity at periphery on both T1 and T2-weighted images. The centre is isointense on T1 and hyperintense on T2-weighted images.
- SWI sequences show multifocal ‘blooming black dots’ mostly in the right side of the brain in keeping with microhaemorrhages.
Diagnosis: Intracerebral haemorrhage caused by cerebral amyloid angiopathy
Discussion:
- Cerebral amyloid angiopathy (CAA) causes 5-20% of all non-traumatic cerebral haemorrhages.
- Advancing age is the stongest risk factor for developing CAA.
- Sporadic CAA usually occurs in patients older than 55 years old.
- Imaging findings may vary depending on the presentation.
- Non-contrast CT scan with acute presentation typically shows a lobar hemorrhage with varying peripheral oedema. Enhancement on contrast-enhanced CT scan is rare.
- MR signal intensity of CAA-associated hemorrhage varies with clot age.
- In addition to residual lobar hemorrhage, T2* (GRE or SWI) sequences demonstrate multifocal punctate ‘blooming black dots’ in the leptomeninges, cortex and subcortical region. The basal ganglia and cerebellum are relatively spared.
- The major differential diagnosis of CAA is chronic hypertensive encephalopathy. The microbleeds in chronic hypertensive encephalopathy often involve the basal ganglia and cerebellum.
- Hemorrhagic metastasis at the gray-white matter junction can resemble CAA. However, unlike tumour, the microbleeds typical of CAA lack mass effect, peripheral oedema and enhancement.