Clinical:
- A 27 years old lady
- Presented with recent onset seizure and headache
- Otherwise no neurological deficit
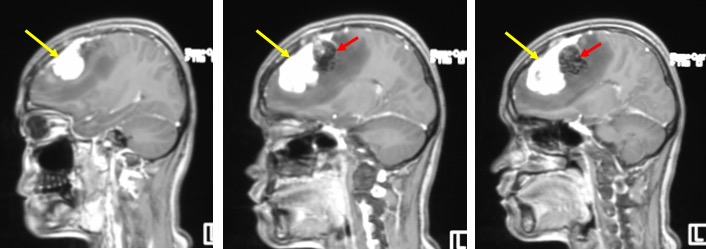
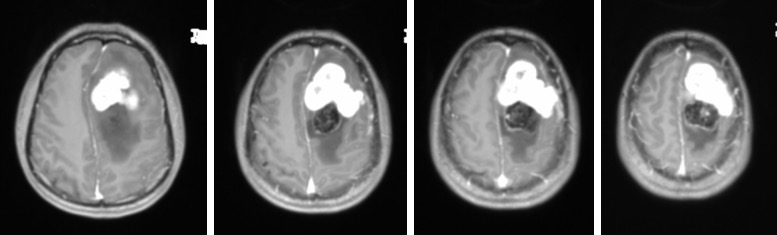
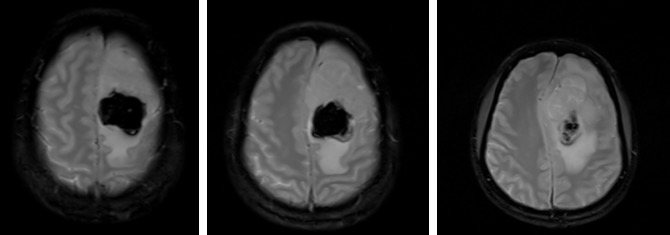
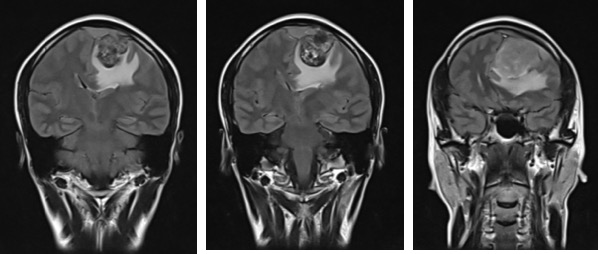
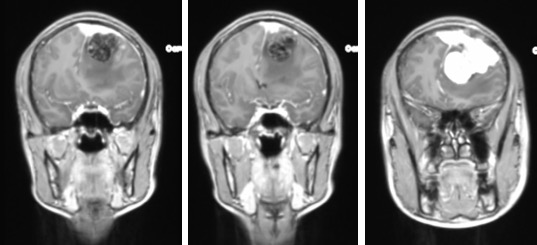
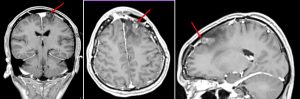
MRI findings:
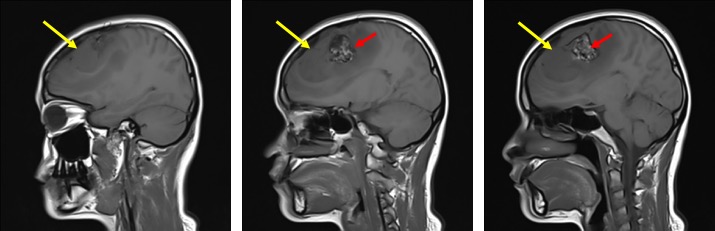
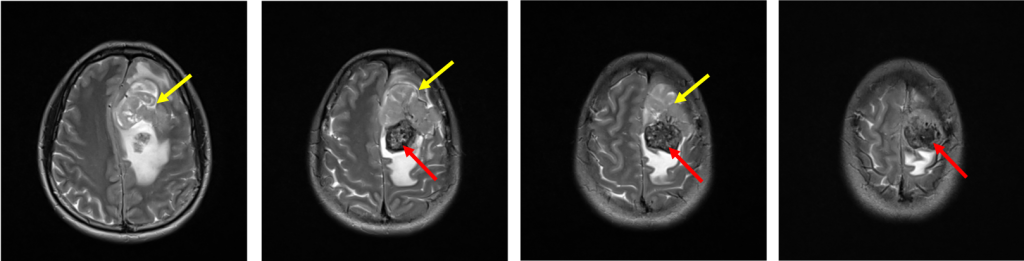
- There is a heterogenous mass at left parasagittal region (yellow arrows)
- It is on hypointense to gray matter on T1WI and iso to hyperintense on T2WI. It shows avid homogenous enhancement post contrast.
- Posterior to the lesion is a rounded lesion which is isointense on T1 and T2WI (red arrows). Prominent flow void regions are seen within it. No enhancement post contrast and blooming artifacts on hemo sequences.
- Dural tail sign is seen.
- There is marked perilesional odema causing midline shift to the right side.
- No hydrocephalus. No other area of leptomeningeal enhancement.
HPE findings:
- Macroscopic: Specimen labeled as tumor and bone
- Microscopic: Section shows fragments of tumour tissue with a few fragments of fibrous tissue, adipose tissue and striated muscle fibres. The tumour cells are in sheets with marked tumour necrosis and focal areas of haemorrhage. Many thin-walled vessels seen and few are dilated. The tumour cells are round to polygonal and exhibit hyperchromatic nuclei with eosinophilic cytoplasm. Mitotic figures are seen (~ 4 per 10 high power field). Sections from the skull bone show cellular ovoid, elongated and spindly neoplastic cell infiltration in some of the marrow spaces. The mitotic count is eight per ten high power field. Prominent vascular slit-like spaces are seen. Psammoma bodies are not seen.
- Immunohistochemical for tumour cells show intense positivity for CD99, BCl-2 and negative staining for EMA and CD34.The CD34 highlights the numerous blood vessels. Ki-67 shows a proliferative index of 40%. For bone specimen shows the neoplastic cells are negative for PR, ER, E-cadherin, Bcl-2, EMA (repeat), Factor VIII, NSE and Synaptophysin. Reticulin staining shows pericellular reticulin staining in most of the tumour cells.
- Interpretation: Hemangiopericytoma with infiltration to bone marrow and pericranium
Diagnosis: Hemangiopericytoma Grade III lesion
Discussion:
- Hemangiopericytoma is also known as meningeal hemangiopericytoma
- Previously it is also called ‘angioblastic meningioma’.
- It is a highly cellular and vascularized mesenchymal tumour and almost always attached to dura. Commonly involve falx, tentorium or dural sinuses.
- It mimics meningioma however no calcification or hyperostosis seen.
- It shows marked enhancement and dural tail seen in about 50% of cases.
- It commonly occurs in 4th to 6th decades, mean age is 43 years.
- Size of lesion is variable; 2-9 cm, mostly >4 cm.
- On CT scan seen as hyperdense extra axial mass with surrounding oedema. Low density cystic or necrotic areas are common. No calcification or hyperostosis.
- MRI on T1WI may be isointense to gray matter with areas of flow void. T2WI heterogenous isointense mass with prominent flow voids, surrounding oedema and typical mass effect. Post contrast shows marked enhancement, often heterogenous and central necrosis may be seen.
- May be indistinguishable with meningioma. Lymphoma and dural metastasis may show similar radiological features but more commonly multifocal and flow voids are absent.
Progress of patient:
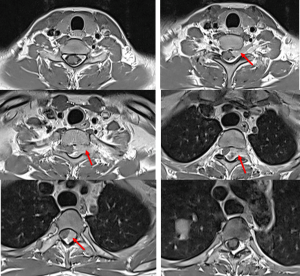
- Presented again 3 years after treatment with complaint of back pain and weakness
- MRI shows a small lesion in the brain suggestive of recurrence and metastasis to spine