Case contribution: Dr Radhiana Hassan
Clinical:
- A 45 years old man
- Underlying DM on medication
- History of being admitted for septic shock secondary to pneumonia
- CT scan brain done due to poor GCS with incidental finding of suprasellar mass
- Referred for further management
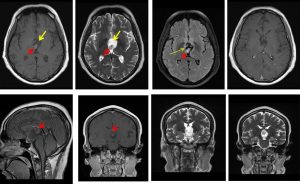
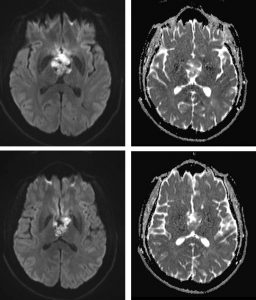
MRI findings:
- A large complex cystic mass is seen at the suprasellar region (yellow arrows).
- Non-enhancing solid components are noted within (red arrows).
- No meningeal enhancement or significant perilesional oedema is noted.
- No blooming artefact is detected on GRE sequence to suggest hemosiderin or calcification.
- The mass is seen extending and expanding the 3rd ventricle, especially the anterior part.
- The adjacent structures such as the optic nerves, optic chiasm, cavernous sinuses and pituitary gland are still preserved. The nearby vessels (bilateral MCA, ACA, terminal ICA) are also unremarkable.
- Grey and white matter differentiation is preserved. No midline shift. No hydrocephalus
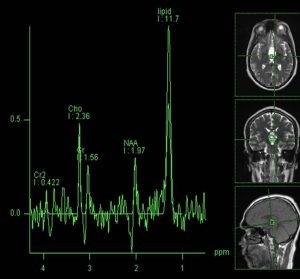
MR spectroscopy shows a large lipid peak characteristic of the cholesterol and lipid constituents found in craniopharyngiomas.
Intra-operative findings:
- Thick-walled encapsulated tumour between optic chiasm and optic tract
- Central debulking done, pale greyish glutinous tumour debulked
- Deroofing done as thick wall adhered strongly to adjacent structures
HPE findings:
- Macroscopy: specimen labelled as cystic tumour and cystic wall
- Microscopy: sections shows predominantly keratin flakes with a focus of bony tissue. Foci of epithelial lining with wet keratin is observed. No calcification. Section of the cyst wall focally lined by squamous epithelium and in areas the lining is replaced by aggregates of foamy macrophages. The wall is composed of aggregates of foamy marophages, multinucleated giant cells, cholesterol cleft and lymphoid aggregate. No calcification seen.
- Interpreation: ovearall features are consistent with craniopharyngioma, WHO Grade 1.
Diagnosis: Craniopharyngioma
Discussion:
- Craniopharngioma is a benign often partially cystic sellar tumour
- There are 2 types; adamantinomatous and papillary type
- Bimodal distribution: peak at 5-15 years and >50 years
- Surgically divided into 3 locations; sellar, prechiasmatic or retrochiasmatic.
