Case contribution: Dr. Radhiana Hassan
Clinical:
- A 75 years old lady
- Para 5, post menopausal not on HRT
- Had hypertension and DM on medication
- Presented with enlarging abdominal mass of one month
- Associated with altered bowel habit
- Colonoscopy shows external compression, otherwise normal finding
- Ultrasound shows uterine lesion
- Hysteroscopy and EUA done, unable to visualize the cervix, hysteroscope able to pass 3cm the cervical rim, endometrial cavity not seen and both ostium not visualized
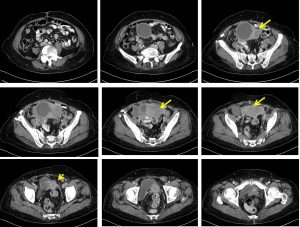

CT scan findings:
- Uterus is anteverted and enlarged.
- An enhancing solid-cystic pelvic mass is visualised within the uterus (yellow arrows).
- No internal septation or intralesional calcification within the cystic component.
- Multiple tiny calcifications are seen within the solid component of the mass.
- There is a poor demarcation between the mass to the uterine fundus, rectum and lower sigmoid colon.
- Clear fat plane demarcation between the mass to the adjacent urinary bladder.
- At the right adnexa, there is a separate cystic lesion measuring 4.6 x 2.6 x 2.6cm, likely right ovary. At the left adnexa, there is also separate cystic lesion measuring 4.0 x 2.7 x 3.1cm, likely left ovary.
- Multiple abdomino-pelvic nodes are noted (less than 1 cm in short axis diameter, SAD)
- No intra-abdominal collection or ascites.
HPE findings:
- Macroscopy: specimen labelled as uterus, falloian tubes and ovaries shows enlarged and distorted uterus. Multiple tumour deposits at surface of uterus, fallopian tubes and ovaries. Cut section of uterus shows extensive tumour arising from endometrium and involving whole thickness of myometrium measuring 170x160x80 mm. The tumour extends to serosa and into the lower uterine segment and cervix. The tumour has tan cut surface with large cystic degeneration at the fundus. Foci areas of necrosis also seen within the tumour. The right and left parametria are involved. Ostia are obstructed by tumour. Multiple cystic dilatation of right fallopian tube and gross distension of left fallopian tube. Cut section of right and left ovaries show tumour infiltration almost the whole tissues.
- Microscopy: endometrioid carcinoma of uterine corpus FIGO Grade 2, TNM stage pT3b pNxpM1 with involvement of both parametria and adnexae, lymphovascular and perineural invasion. Metastatis adenocarcinoma of peritoneal nodule at upper rectum, omentum, appendix and peritoneum. No nodal metastasis
Diagnosis: endometrial cancer (endometrioid adenocarcinoma) with metastasis
Discussion:
- Most endometrial cancers are adenocarcinomas, and endometrioid cancer is the most common type of adenocarcinoma
- The grade of an endometrial cancer is based on how much the cancer cells are organized into glands that look like the glands found in a normal, healthy endometrium.
- Grade 1 tumors have 95% or more of the cancer tissue forming glands.
- Grade 2 tumors have between 50% and 94% of the cancer tissue forming glands.
- Grade 3 tumors have less than half of the cancer tissue forming glands. Grade 3 cancers tend to be aggressive (they grow and spread fast) and have a worse outlook than lower-grade cancers.
- FIGO staging for endometrial cancers:
- Stage 0-carcinoma in situ
- Stage I-limited to the body of the uterus
- Ia: no or less than half (≤ 50%) myometrial invasion
- Ib: invasion equal to or more than half (≥ 50%) of the myometrium
- Stage II-cervical stromal involvement
- Stage III- local or regional spread of the tumor
- IIIa: tumor invades the serosa of the body of the uterus and/or adnexa
- IIIb: vaginal or parametrial involvement
- IIIc: pelvic or para-aortic lymphadenopathy
- Stage IV-involvement of rectum and or bladder mucosa and or distant metastasis
- IVa: bladder or rectal mucosal involvement
- IVb: distant metastases, malignant ascites, peritoneal involvement
