Case contribution: Dr Radhiana Hassan
Clinical:
- A 7 years old girl with underlying epilepsy
- Presented with status epilepticus
- Initially she was intubated for 2 days, poor recovery after extubation
- Fluctuation in GCS with bilateral hypertonia. Babinski upgoing bilaterally.
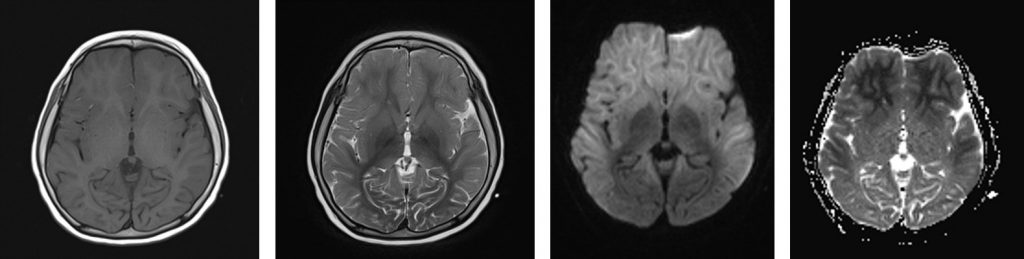
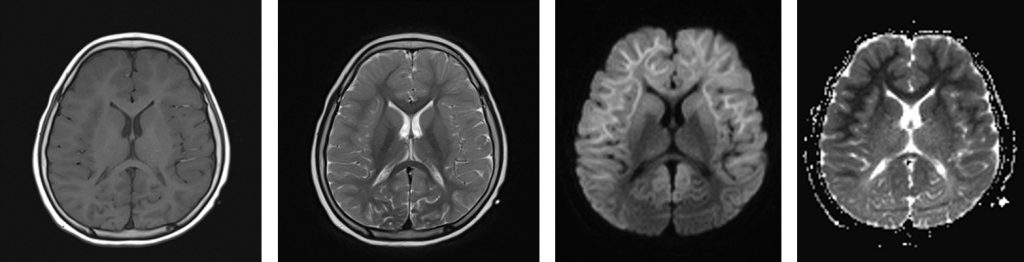
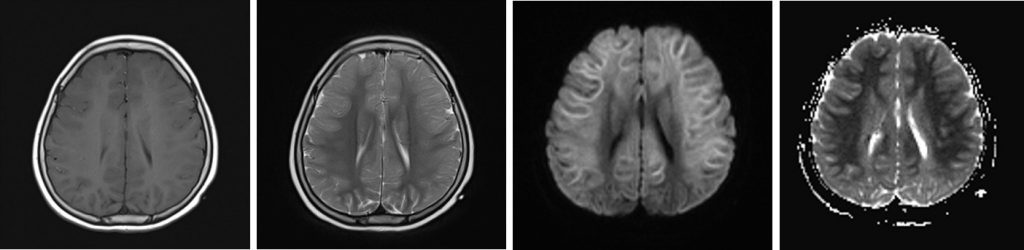
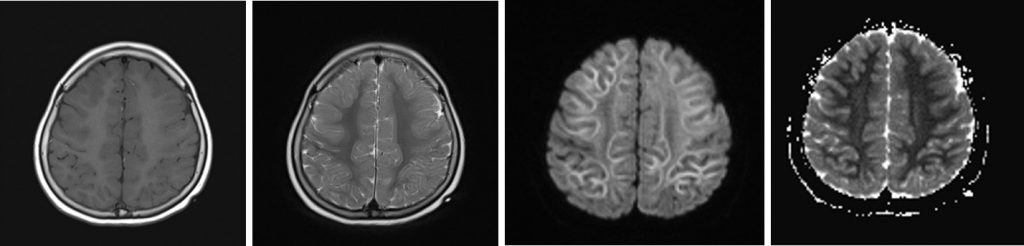
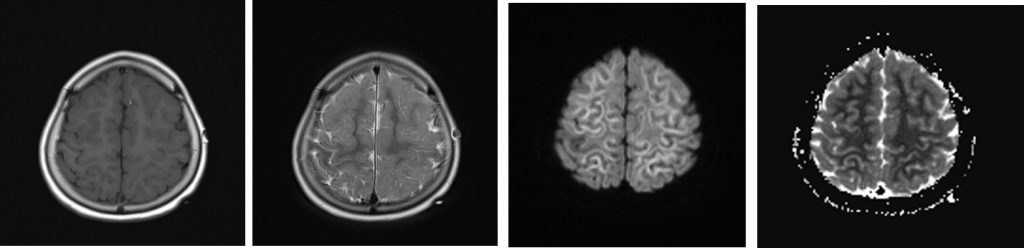
MRI findings:
- There is extensive subcortical white matter restricted diffusion involving frontotemporoparietal lobe with symmetrical distribution bilaterally
- Relative sparring of the occipital lobe is seen
- No corresponding hyperintensity on T2/FLAIR sequences
- Mild effacement of cerebral sulci at both frontal region
- No abnormal enhancing brain lesion
Diagnosis: ALERD (Acute leukoencephalopathy with restricted diffusion)
Discussion:
- Acute encephalopathy refers to acute insult to the brain and presents with seizures, impaired consciousness, and other neurological symptoms.
- Many new entities that cause acute encephalopathy in children have been described such as ADEM, acute necrotizing encephalitis (ANE), fever-induced refractory epilepsy syndrome (FIRES), clinically mild encephalopathy with reversible splenial lesion (MERS), and autoimmune encephalitis
- ALERD is a clinical-radiological syndrome seen in childhood presented as acute encephalopathy with MRI shows areas of restricted diffusion seen in both gray and white matter
- It has been reported mainly from East Asia
- Those occurring in the setting of an infection can be termed as infectious ALERD as similar presentation is seen with toxins such as cranial irradiation, therapeutic agents, and drugs of abuse and environmental toxins where the term toxic ALERD is preferred
- As the name indicates, ALERD is characterized by restricted diffusion on MRI and neuroimaging plays an important role in the diagnosis.
- Computed tomography (CT) scan of the brain is mostly normal unless late in the disease in severe cases, wherein there may be white matter hypodensities.
- Diagnosis is made on the MRI of the brain. The changes on conventional sequences such as T1-W, T2-W, and FLAIR may be subtle, and unless DWIs are acquired, a diagnosis of ALERD can be easily missed.
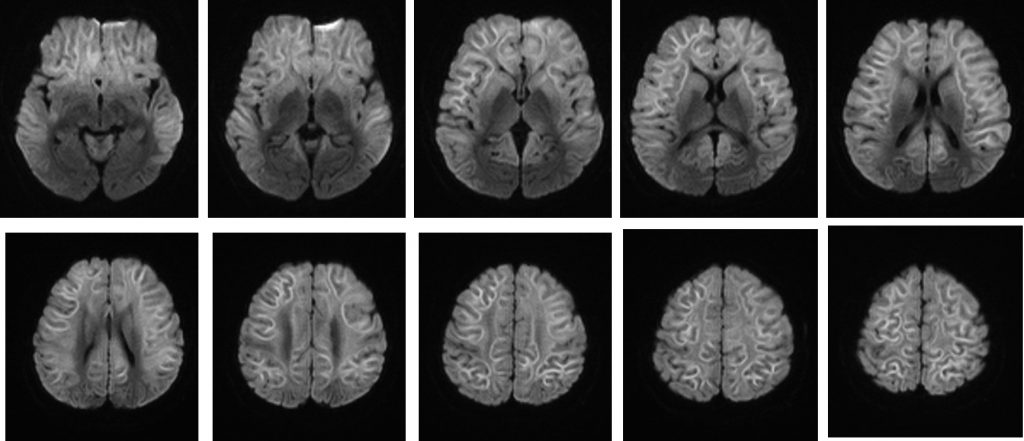
- Two distinct groups according to the distribution of brain lesions have been identified. The one with diffuse areas of restricted diffusion on MRI is called diffuse ALERD and those where there is sparing of the central regions of the brain are called as central-sparing ALERD. The latter is equivalent to the well-described and well-known acute encephalopathy with biphasic seizures and late reduced diffusion (AESD)
- The characteristic “bright tree appearance,” which represents high-signal intensity on DWI in the widespread subcortical white matter, which has the appearance of tree branches.
- Central sparing is defined as a lack of high-signal intensity on DWI in subcortical white matter in the primary sensorimotor areas, while diffuse ALERD involves both the hemispheres in a widespread manner.
- On follow up MRI, mild-to-severe cerebral atrophy seen when the imaging is repeated after 2–4 weeks, and there is resolution of white matter restriction on DWI over 2–4 weeks. Laminar necrosis and increased signal intensities in the subcortical white matter on T2-W images in diffuse lesions can be seen. Hyperintensities can be seen in the caudate nucleus in some patients, whereas rest of basal ganglia, thalami, and corpus callosum are usually spared in ALERD.
- Up to 5%–10% mortality has been reported in diffuse ALERD, while in the central-sparing ALERD/AESD, there have been no reports of death. More than 2/3rd of children with ALERD develop sequelae such as postencephalopathic epilepsy, hyperactivity with language delay, cognitive impairment, spasticity, dyskinesias, and hemiparesis.
