Clinical:
- A 41 years old lady
- No known medical illness
- Presented with sudden onset of headache
- Associated with blurring of vision.
- Clinical examination shows bitemporal hemianopia
- Blood investigations are unremarkable
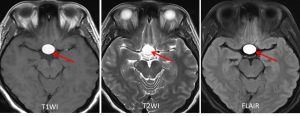

MRI findings:
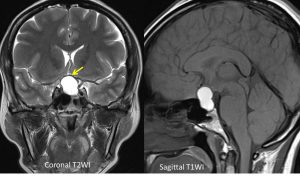
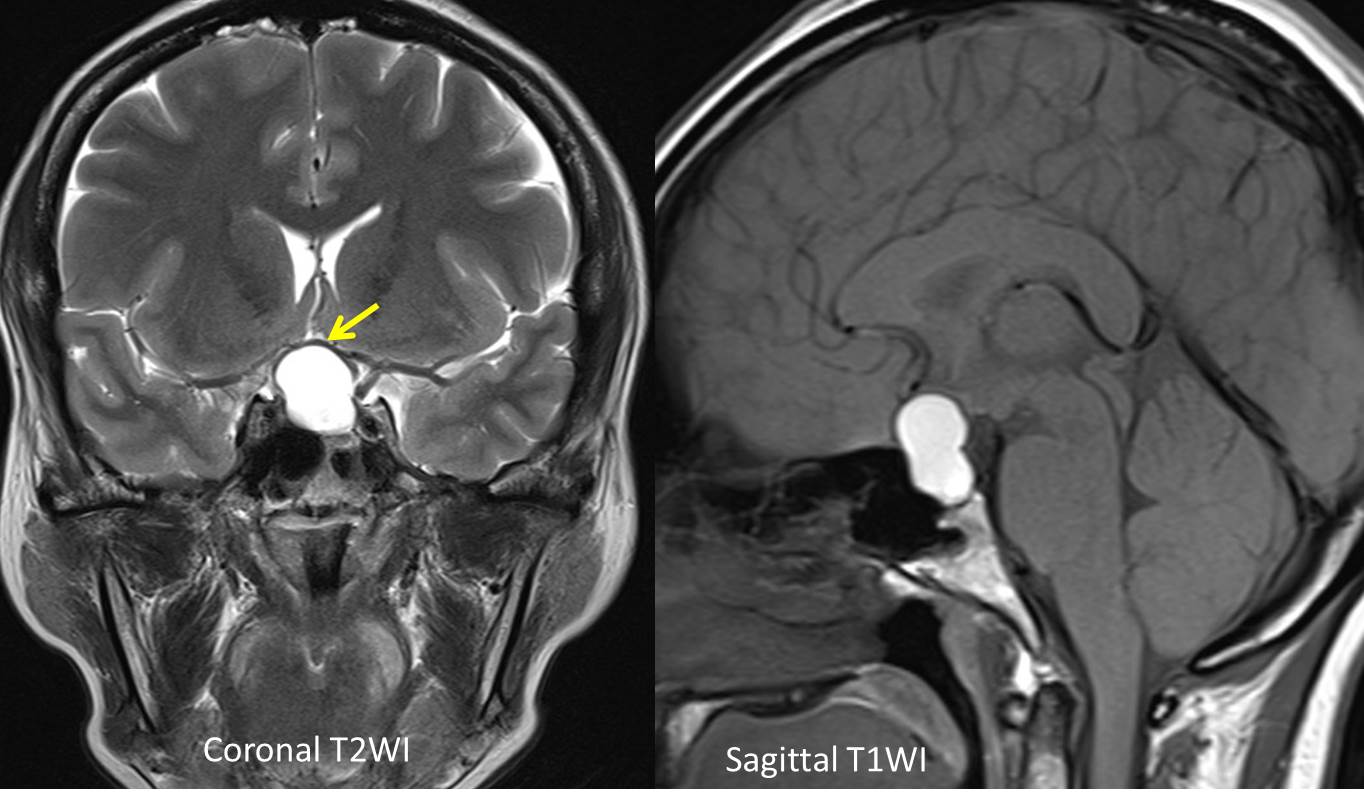
- There is a lobulated lesion at the sellar extending to suprasellar region (red arrows) measuring about 18mm (W) x 15mm (AP) x 20mm (CC).
- It is hyperintense on T1 and T2-weighted image and not suppressed on fat suppression sequence.
- It causes compression and elevation of the optic chiasm (yellow arrow).
- There is no communication with the adjacent intracerebral vessels. Both ICAs are displaced laterally with no significant compression or luminal narrowing seen.
- There is minimal expansion of the sella. The normal pituitary is not seen.
HPE findings:
- Macroscopy: specimen labelled as pituitary tumour, consist of a piece of brownish tissue measuring 3x2x2 mm.
- Microscopy: section shows monomorphic proliferation of cells with uniform round nuclei, delicate stippled chromatin, inconspicuous nucleoli and moderate amount of cytoplasm. Mitosis and necrosis is not seen.
- Interpretation: compatible with pituitary adenoma.
Diagnosis: Pituitary apoplexy
Discussion:
- Pituitary apoplexy is an acute clinical syndrome typically comprises of headache, visual deficits, ophthalmoplegia, and altered mental status
- It is caused by either hemorrhagic or non-hemorrhagic necrosis of the pituitary gland.
- An existing pituitary adenoma is usually present (60-90%) but it can occur with healthy pituitary glands
- Pituitary adenomas are very common pituitary tumour and are often not diagnosed.
- MRI is the best imaging modality to demonstrate mass lesion in the sella and abnormal signal intensity suggestive of hemorrhage (T1-hyperintense) as demonstrated in this case.
Progress of patient:
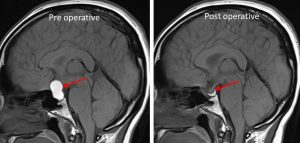
- Transphenoidal tumour resection done
- Review 2 months after surgery showed improvement in vision
- No more headache
Recent Comments