Case contribution: Assoc. Prof. Dr Hilwati Hashim
Clinical:
- A 29-year-old male
- Presented with a 1 day history of lethargy and reduced responsiveness associated with slurred speech.
- It was preceded with a 3 days history of fever.
- On examination, his Glasgow Coma Scale (GCS) was 10/15.
- His CVS examination revealed a heart murmur.
- His white cell count (WCC) was 22.0.
- The blood culture result came back positive for MSSA.
- An Echocardiogram was performed and showed presence of vegetations on the mitral and aortic valves.
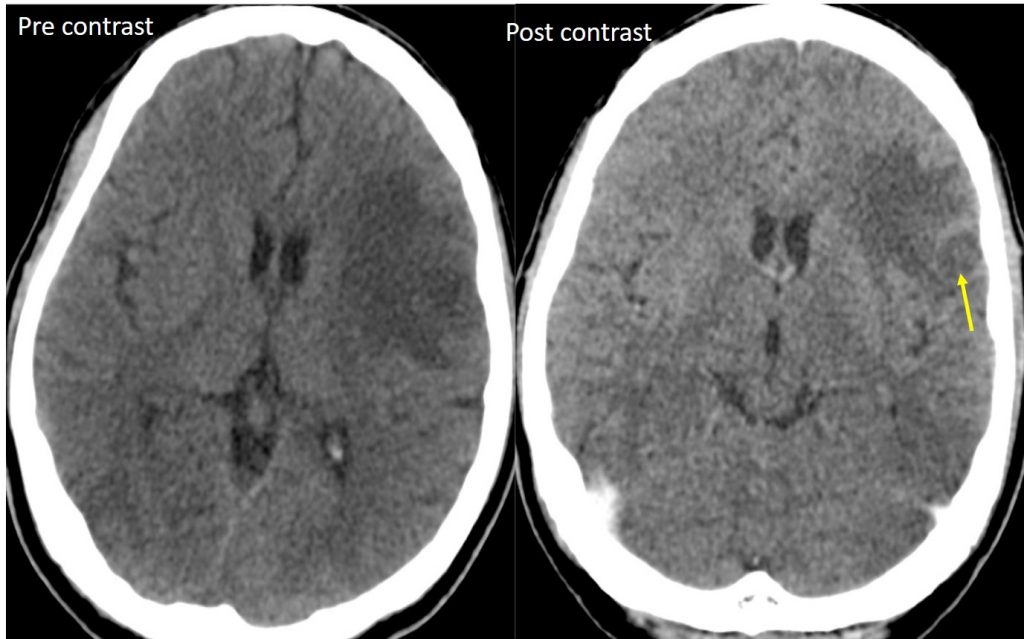
CT scan findings:
- There is an ill defined ring-enhancing lesion in the left frontal lobe
- There is associated perilesional oedema.
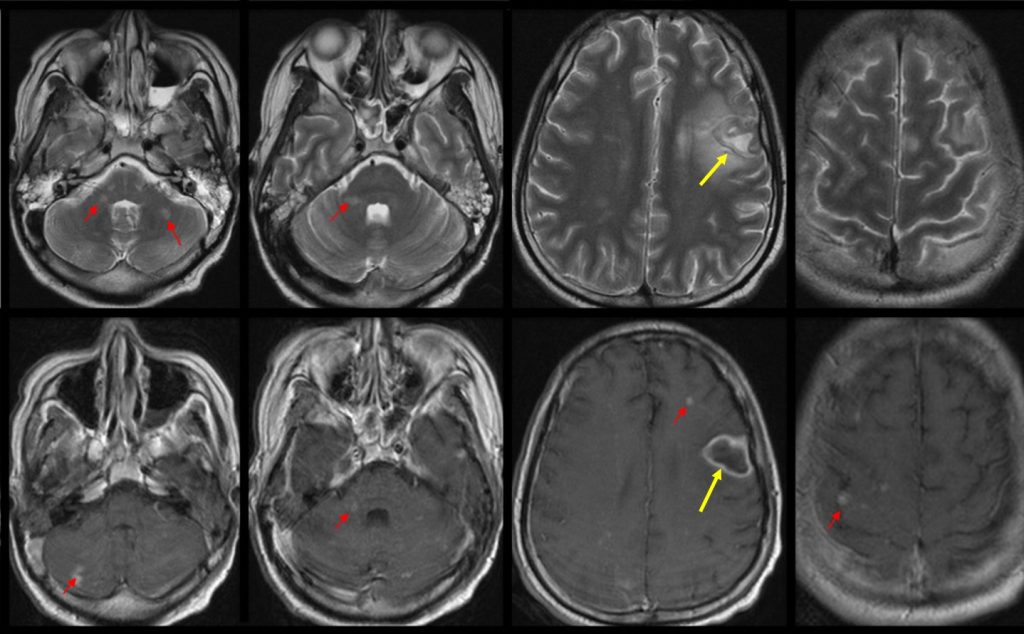
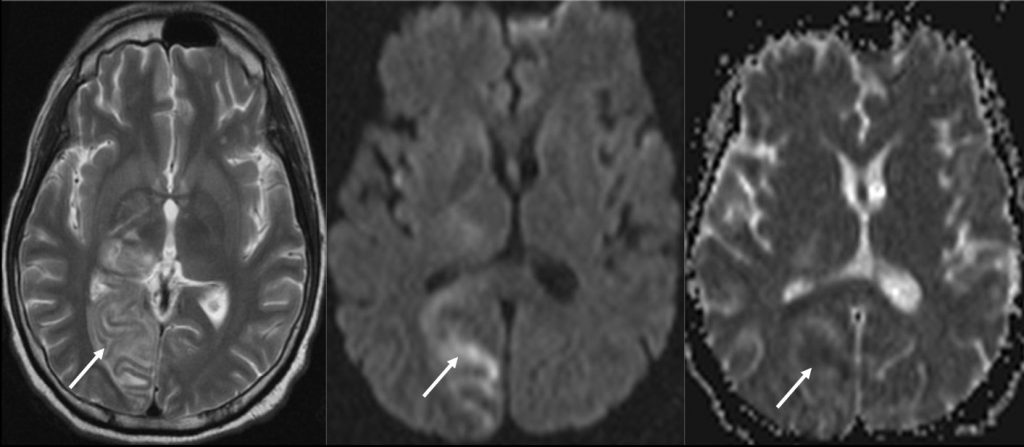
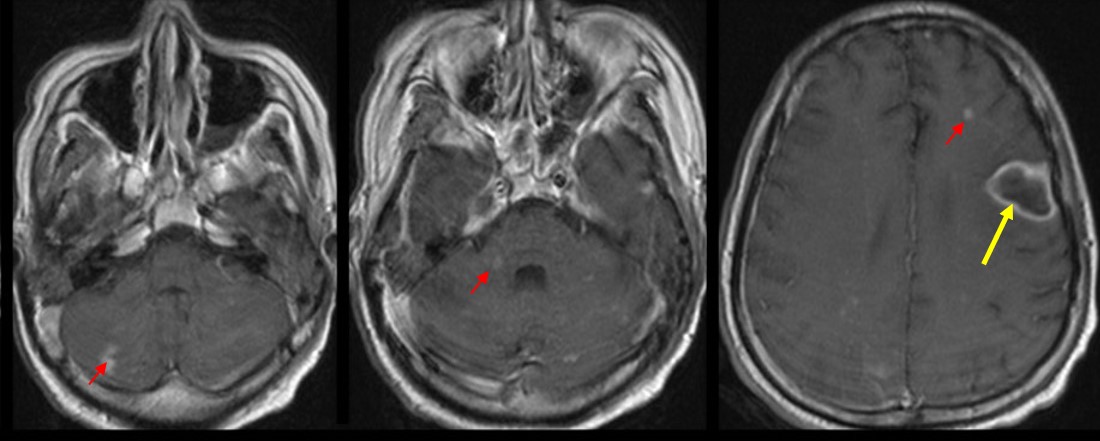
MRI findings:
- The left frontal lesion (yellow arrows) has a hypointense wall on T2 with hyperintense central core. Post contrast, the lesion has a thin wall, ring enhancing pattern suggestive of an abscess. Perilesional oedema is also seen on the T2W sequence.
- Multiple small foci of T2 hyperintensities scattered in the posterior fossa (cerebellum, middle cerebellar peduncle, pons), grey-white matter junction and cortical area of bilateral cerebral hemispheres. These lesions enhances post contrast. The post contrast sequence also demonstrates multiple other small cortical lesions and lesions at grey white matter junction which are not seen in the T2W sequence (red arrows).
- There is also an area of T2 hyperintensity involving the grey and white matter of the right occipital lobe (white arrows). Some parts of the area demonstrated restricted diffusion (hyperintense on DWI and Hypointense on ADC). This is suggestive of a right PCA territory infarct
Diagnosis: Septic embolic encephalitis
Discussion:
- Infective thromboembolism, usually from bacterial endocarditis, can result in diffuse infection, infarction and haemorrhage.
- The common differential diagnoses for lesions distributed at the grey-white matter junction are metastasis and septic emboli.
- In this case, correlating with the clinical history of reduced consciousness, fever, MSSA positive culture and vegetations on Echocardiogram, septic embolic encephalitis is the most likely diagnosis.
- Although not present in this case, haemorrhage is also seen in septic embolic encephalitis. It includes subarachnoid haemorrhage (SAH), lobar hemorrhages, and hemorrhagic transformation of an ischemic stroke.
Recent Comments