Clinical:
- A 20-year old man without any known medical illness
- Suddenly had fits at home.
- Brought in unconscious to ED
Imaging findings:
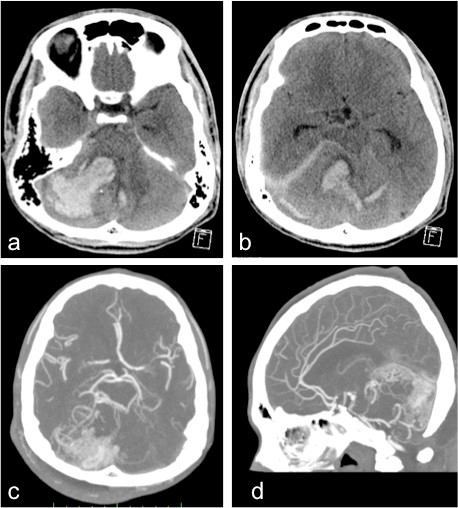
- Axial non-contrasted CT scan of the brain with soft tissue window (a,b) shows an intracerebral hemorrhage in the cerebellum; more on the right side with intraventricular extension.
- A few punctate foci of calcifications were also seen adjacent to the region of hemorrhage.
- Mild dilatation of both temporal horns of the lateral ventricle is seen.
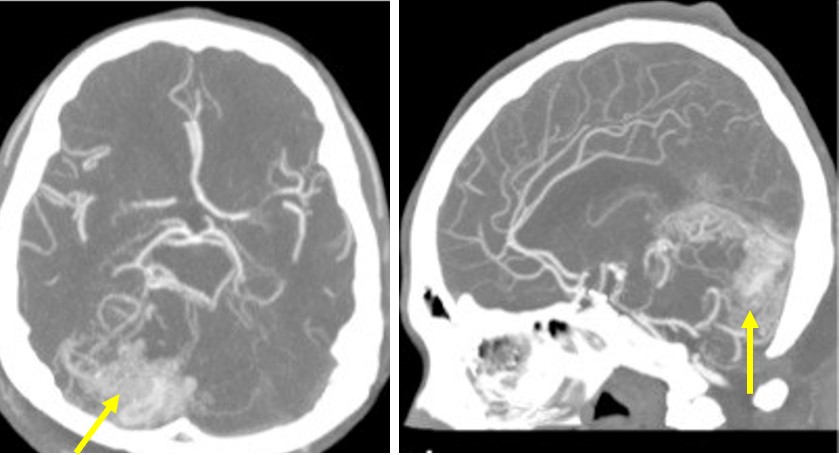
- CT angiogram MPR in axial and sagittal (c,d) showed multiple dilated vessels in the posterior fossa region.
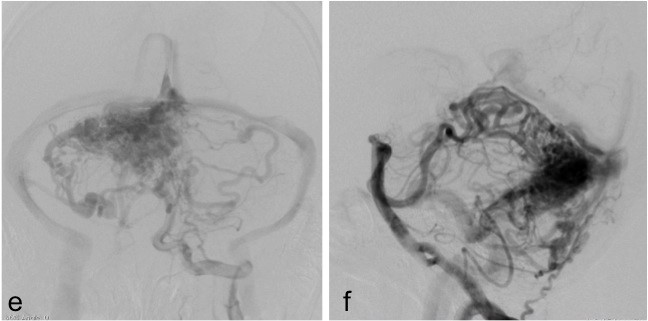
- Digital subtracted cerebral angiogram in frontal and lateral views (e,f) confirmed the presence of nidus, feeding vessels and dilated veins consistent with an arteriovenous malformation in the posterior fossa.
Diagnosis: Ruptured cerebral arteriovenous malformation.
Discussion:
- Cerebral arteriovenous malformation occur in about 0.1-4% of population but become symptomatic in only 12% of affected individuals.
- There is no gender predilection.
- It tends to be solitary in majority of cases.
- Posterior fossa arteriovenous malformation occurs in 15% of AVMs.
- The annual incidence of hemorrhage of unruptured and untreated brain AVMs is 2-4%. Following hemorrhage, the risk of further bleed in the next 12 months is up to 18%.
- In bleeding AVMs, parenchymal is more common than intraventricular or subarachnoid hemorrhage.
- Calcification is noted in 25-30% of cases.
- On contrasted CT or MRI, enlarged feeding arteries, nidus of tightly packed; enlarged vessels and dilated draining veins can be demonstrated.
- The digital subtracted angiography remains the gold standard imaging technique. It is able to delineate the angio-architexture of the lesion.
Recent Comments