Clinical:
- A 68 years old male
- Presented with painless per rectal bleeding for one day
- No anaemic symptoms
- History of altered bowel habit for 4 months and constitutional symptoms for 2 months
- Clinical examination is unremarkable.
- Colonoscopy done shows external compression at rectum from external wall, smooth normal mucosa, erythema with presence of dilated vessels.
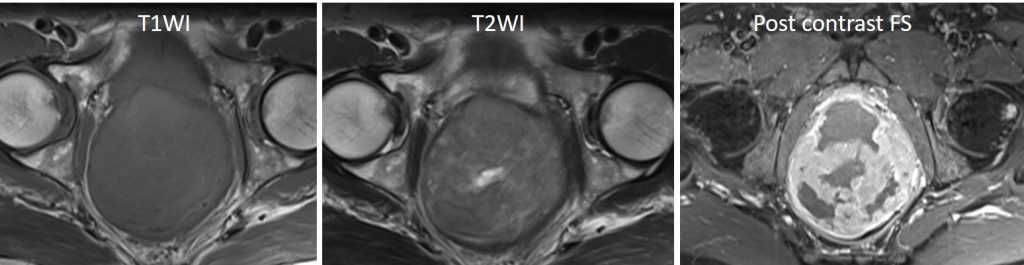
MRI findings:
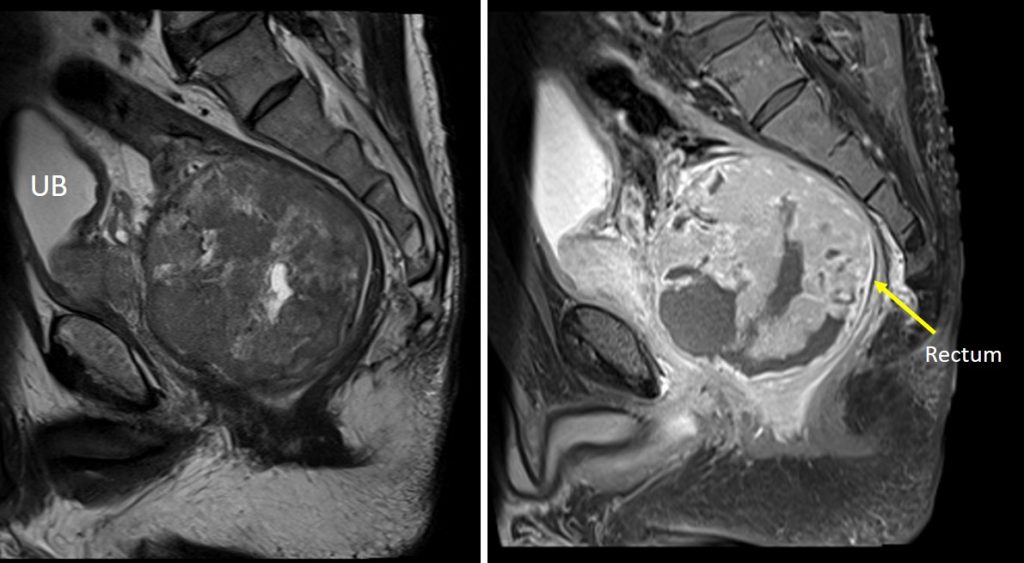
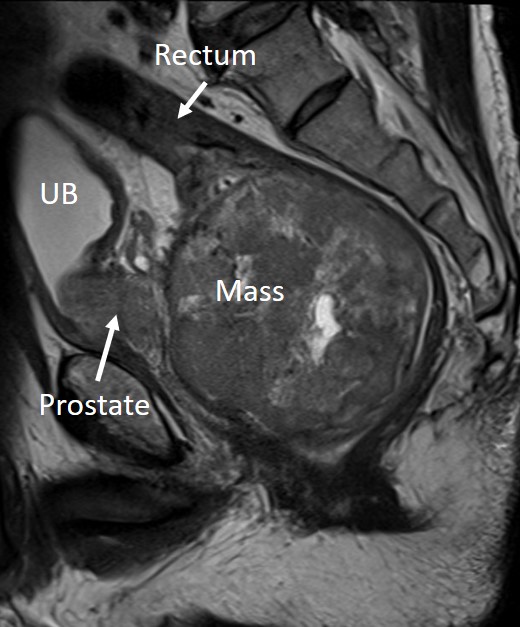
- There is a large well-demarcated round pelvic mass seen arising from the anterior wall of the rectum. It measures about 8.8 AP x 8.8 W x 8.9 cm CC.
- It is a soft tissue mass which mainly shows hypointense signal on T1 and heterogenous signal on T2, with areas of necrosis. Heterogenous enhancement is noted post gadolinium.
- No signal void areas seen to suggest intralesional calcification.
- The mass is extraluminal and compresses the rectal lumen causing luminal stenosis; starting about 2.3 cm from the anal verge with total collapse @ stenosis about 11.3 cm in length. However, the proximal bowel is not dilated.
- The mass is seen pushing the prostate and seminal vesicles anteriorly with clear fat plane seen in between.
HPE findings:
- Macroscopy: specimen labelled as pelvic mass
- Microscopy: section shows 1 strip of viable tumour tissue and 3 strips of necrotic tissue. The tumour consists of spindle cell proliferation. The spindle cells display mildly pleomorphic, hyperchromatic to vesicular nuclei with inconspicuous nucleoli. No mitosis seen. Scattered small blood vessels are noted.
- Immunohistochemical studies shows the spindle cells are CKAE1/AE3 and S100 negative
- Impression: gastrointestinal stromal tumour (GIST)
Diagnosis: Rectal GIST
Discussion:
- GISTs originate at any location along the gastrointestinal tract, most frequently in the stomach (60%), followed by the small bowels (jejunum and ileum:30%, duodenum: 4–5%).
- Rectal GIST comprises about 4% of all total GISTs.
- Imaging findings depends on size and location of tumour.
- The tumours are often exophytic.
- The enhancement is peripheral with areas of necrosis
- Calcification is uncommon (3%).
- The presence of necrosis, hemorrhagic and cystic change make appearances variable on MRI.
Progress of patient:
- Tumour resection done.
- Final HPE diagnosis, GIST, spindle cell type, moderate risk.
- Referred to oncologist for further treatment.
Recent Comments