Clinical:
- A 70 years old man
- No known medical problem
- A smoker
- Presented with abdominal mass for one year
- Dizziness for 3 days
- Went to GP and noted to have high BP

Radiographic findings:
- There is homogenous opacity lateral to lumbar spine on the left side
- The opacity shows smooth convexity with fairly well defined lateral border (yellow arrows)
- No obliteration of left psoas outline
- Minimal displacement of bowel loops peripherally

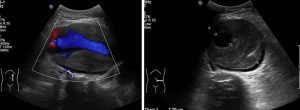
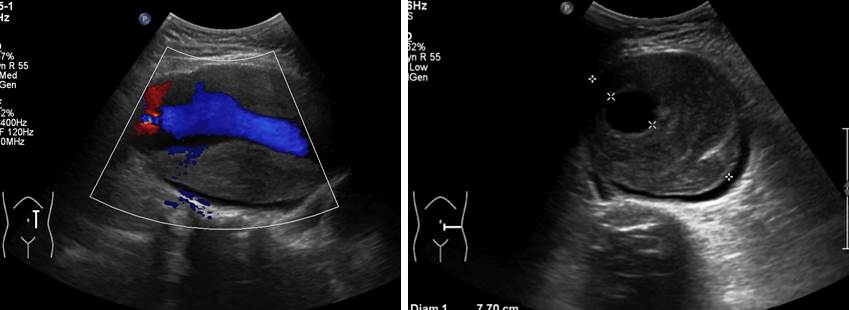
Ultrasound findings:
- Dilated abdominal aorta is seen from the level of superior mesenteric artery until the level of aortic bifurcation. The common iliac arteries are not dilated.
- The diameter of abdominal aorta at the level of coeliac trunk and superior mesenteric artery measures 2.9 cm and 3.4 cm respectively.
- The infra-renal abdominal aorta is much dilated and torturous; widest diameter of 8.1 cm. Thick luminal thrombus causing approximately 70% luminal stenosis. The true lumen measures 2.3 cm.
- A sliver of fluid surrounding the posterior aspect of the thrombus is seen which suggest presence of a small intramural hematoma. However no definite flap is identified to indicate presence of dissection.
- No free fluid in the abdominal cavity or in the retroperitoneal space to suggest aortic leak.
Diagnosis: Abdominal aortic aneurysm with no feature of leaking or dissection.
Discussion:
- Abdominal aortic aneurysms are focal dilatations of the abdominal aorta measuring 50% greater than the proximal normal segment, or >3 cm in maximum diameter.
- Fusiform type aneurysm is more common than saccular aneurysm.
- Males are much more commonly affected than females (4:1 male/female ratio)
- Ultrasound is optimal for general AAA screening and surveillance, The sensitivity and specificity approach 100%; however, it should be noted that visualization is poor in 1% to 3% of patients due to patient habitus or overlying bowel gas.
- However, ultrasound does not provide sufficient detail for procedural planning or more complex lesions. Ultrasound cannot be reliably used in evaluation for endovascular treatments and assessment of regional branch vessels.
- Intervention is usually performed if
- Diameter >5.5 cm
- enlargement in transverse diameter ≥5 mm in 6 months
- Symptomatic lesion
Recent Comments