Clinical:
- A 43 years old lady
- No known medical illness
- Presented with recent onset seizures
- No body weakness
- No constitutional symptoms
MRI findings:
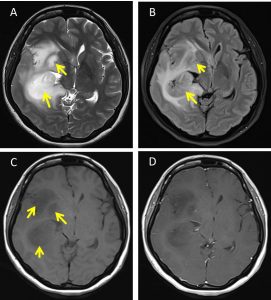
- MRI brain in (A) T2WI, (B) FLAIR, (C) T1WI and (D) T1+Gadolinium sequences
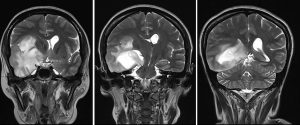
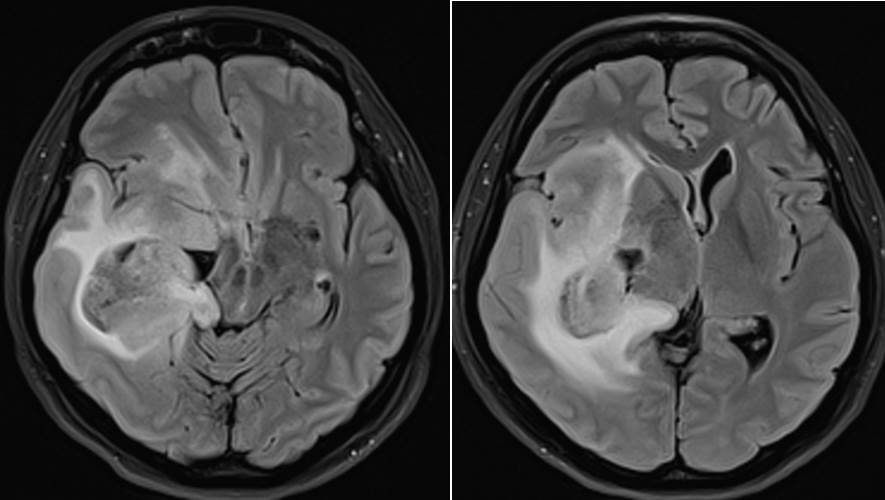
- There are intra-axial masses identified within the right frontotemporal region (yellow arrows) involving the right basal ganglia
- These masses appear hypointense on T1, hyperintense on T2 and slightly hyperintense on FLAIR sequences. No enhancement on post contrast images.
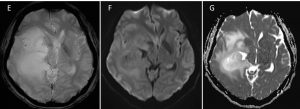
- No blooming artefact is identified on HEMO sequence (E) to suggest presence of blood product/ calcification.
- No area of restricted diffusion is observed on DWI/ADC sequences (F &G).
- There is minimal perilesional vasogenic oedema, effacement of the right lateral and 3rd ventricles. Compression effect causing distortion of the midbrain is also seen.
- Midline shift to the left of 1.0 cm is observed. No hydrocephalus observed.
HPE findings:
- Macroscopy: specimen labelled as brain tumour consists of multiple pieces of whitish tissue
- Microscopy: sections from the specimen shows fragments of tumour tissue composed of moderately cellular cells in a background of loosely structured microcytic stroma. The tumour cells exhibit mild nuclear atypia which are enlarged, cigar-shaped nuclei with irregular hyperchromatic nuclei and scanty cytoplasm. No mitosis, necrosis or microvascular proliferation seen. No normal brain tissue identified in this biopsy.
- Immunohistochemical studies shows the tumour cells are GFAP positive and Ki67 proliferative index 4%.
- Interpretation: Diffuse astrocytoma, WHO Grade II.
Diagnosis: Diffuse astrocytoma.
Discussion:
- Also known as Grade II astrocytoma or low grade astrocytoma
- It is a primary brain tumour of astrocytic origin with intrinsic tendency for malignant progression, degeneration into anaplastic astrocytoma.
- A well-differentiated but infiltrating neoplasm with slow growth pattern
- Majority presented between 20-45 years old
- Seizure is the most common presenting feature
- Supratentorial location in 2/3 of cases and infratentorial in 1/3 of cases
- Variable in size
- It may extend into cortex, 20% involve deep gray matter structures such as thalamus and basal ganglia
- NECT: Ill-defined hypodense/isodense mass, calcification in 20% of cases, cystic component is rare.
- CECT: no enhancement or very minimal
- T1-MRI: homogenous hypointense mass which may expand white matter and adjacent cortex, appears circumscribed but infiltrates adjacent brain, calcification and cysts are uncommon
- T2-MRI: homogenous hyperintense mass with infiltration to adjacent brain, may expand adjacent cortex, hemorrhage and surrounding oedema are rare
- FLAIR: homogenously hyperintense mass
- DWI: no restricted diffusion
- T1+Gadolinium: usually no enhancement, enhancement suggests progression to higher grade
- MRS: high choline, low NAA typical but not specific
- Median survival: 6-10 years.
Recent Comments