Case contribution: Dr Radhiana Hassan
Clinical:
- A 22 years old lady
- No known medical illness
- Progressive abdominal distension for few months
- No compressive symptoms
- No constitutional symptom
CT scan findings:
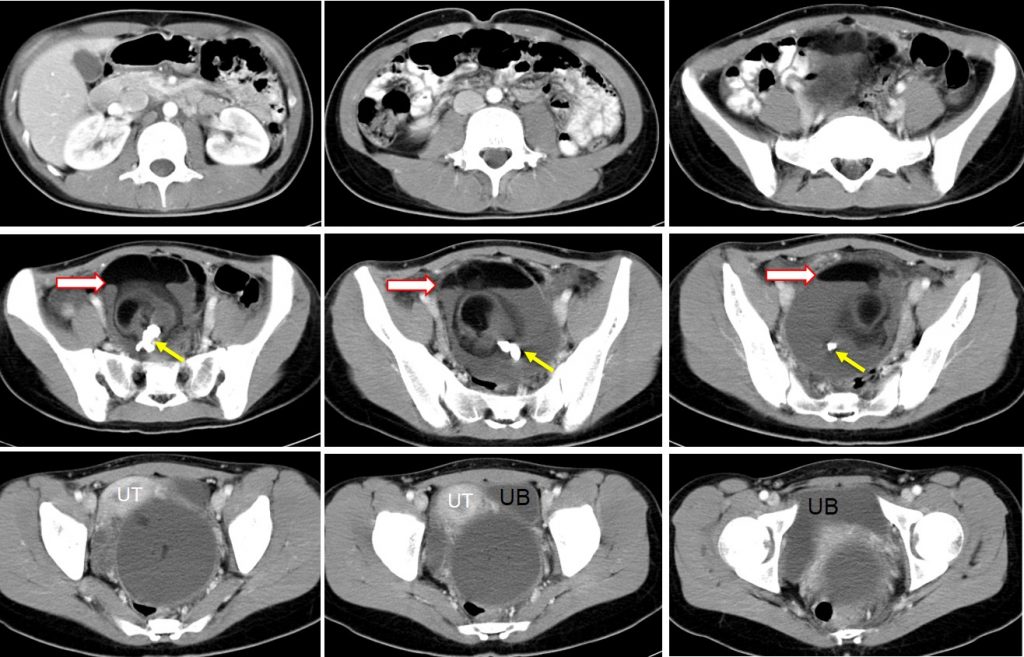
- A large mass measuring 11x9x12 cm arising from left ovary
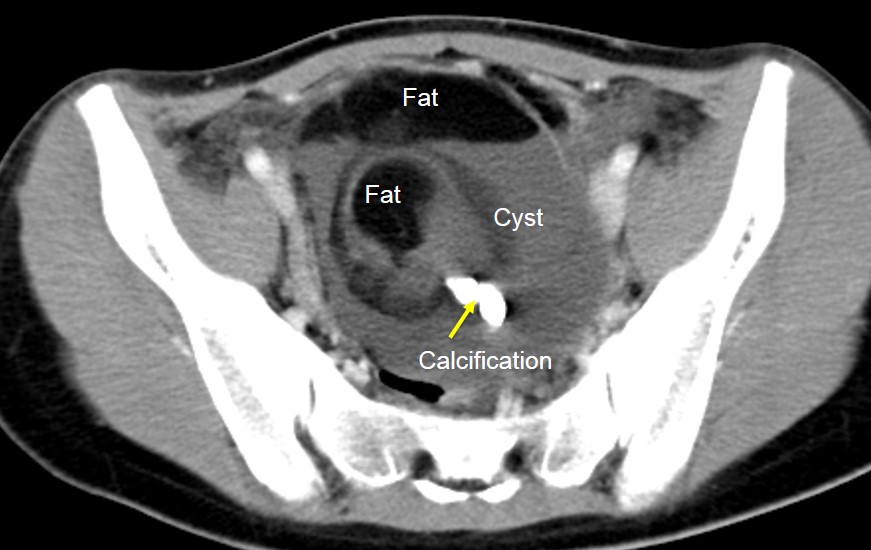
- The lesion is mainly cystic in density
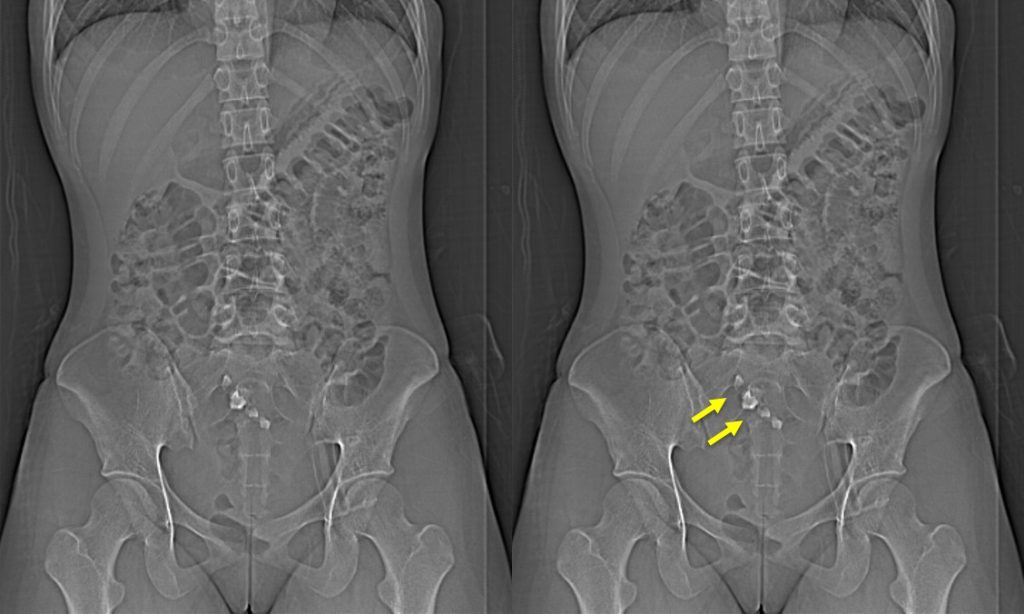
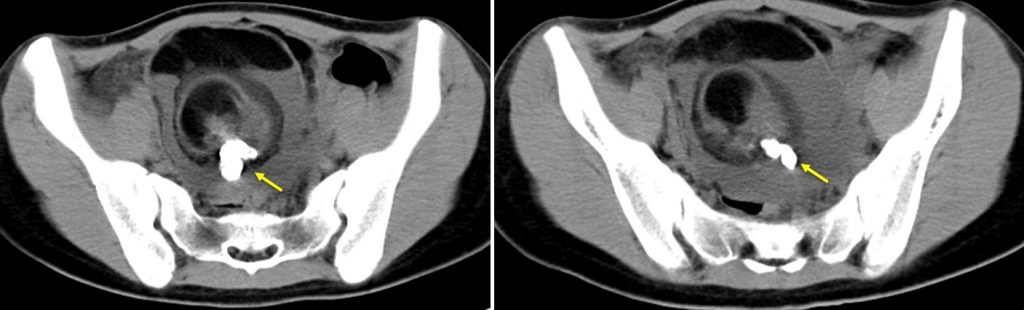
- There are calcifications within the lesion (yellow arrows), on CT scanogram seen as tooth configuration
- There is fat component within the lesion with fat-fluid level seen (block arrow)
- The uterus is anteriorly displaced.
- The mass also compresses the bladder and the rectum.
- There is no ascites.
Intra operative findings:
- Left ovarian cyst. Not twisted.
- Free tubal end of left fallopian tube
- Right ovary and right fallopian tube is normal
- Uterus is normal in size.
HPE findings:
- Macroscopy: specimen labelled as left ovarian cyst consists of a partially ruptured cystic mass measuring 90x85x70mm. Cut section shows a uniloculated cyst with the wall thickness of 1-3 mm. There is a solid area measuring 55x50x45 mm with attached tooth. Clumps of hair is also seen.
- Microscopy: sections of the ovarian cyst wall show areas lined by stratified squamous epithelium. In other areas, the epithelial lining is lined by foamy macrophages and chronic inflammatory cells. The solid area has epidermis with dermis and underlying adnexal structures, subcutaneous adipose tissue, glial tissue, nerve bundles and cartilage. No immature element or malignancy seen.
- Interpretation: mature cystic teratoma.
Diagnosis: Mature ovarian teratoma
Discussion (calcification within ovarian lesion):
- Ovarian calcifications are considered dystrophic (associated with cellular degeneration).
- Ovarian calcifications are commonly found in the context of a mass (mature teratoma, mucinous cystadenoma, serous neoplasia) but also in grossly normal ovaries (mostly within corpora albicantia).
- The pathophysiology: Impaired metabolism elevates the pH and induces intracellular precipitation of calcium salts within epithelial cells or hystiocytes. Large extracellular calcifications result from fused calcific bodies which have been extruded from calcified cells.
- It is often identified by radiologists on ultrasound or other pelvic imaging modalities.
- Radiological descriptions used for pelvic calcifications include curvilinear or punctate echogenic foci, usually between 1 – 3 mm, “Popcorn” calcifications in uterine fibroids, rim-like calcifications in ovarian cystic lesions or sometimes uterine fibroids and appearance of a tooth or other bone (e.g. clavicle) in dermoid cysts.
- By itself, ovarian calcification is not an indication for biopsy or oophorectomy; pathologic evaluation of calcifications is usually seen in the setting of a mass or in prophylactic oophorectomies.
- Histologically, calcifications are divided into psammomatous (psammoma bodies) and nonpsammomatous. Identifying psammomatous calcifications is important; their presence in an otherwise normal ovarian specimen should raise the possibility of an underlying serous neoplasm and prompt additional sampling and correlation with intraoperative findings
Recent Comments