Case contribution: Dr Radhiana Hassan
Clinical:
- A 65 years old man
- Presented with chronic cough
- Associated with loss of appetite and loss of weight
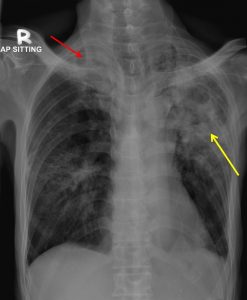
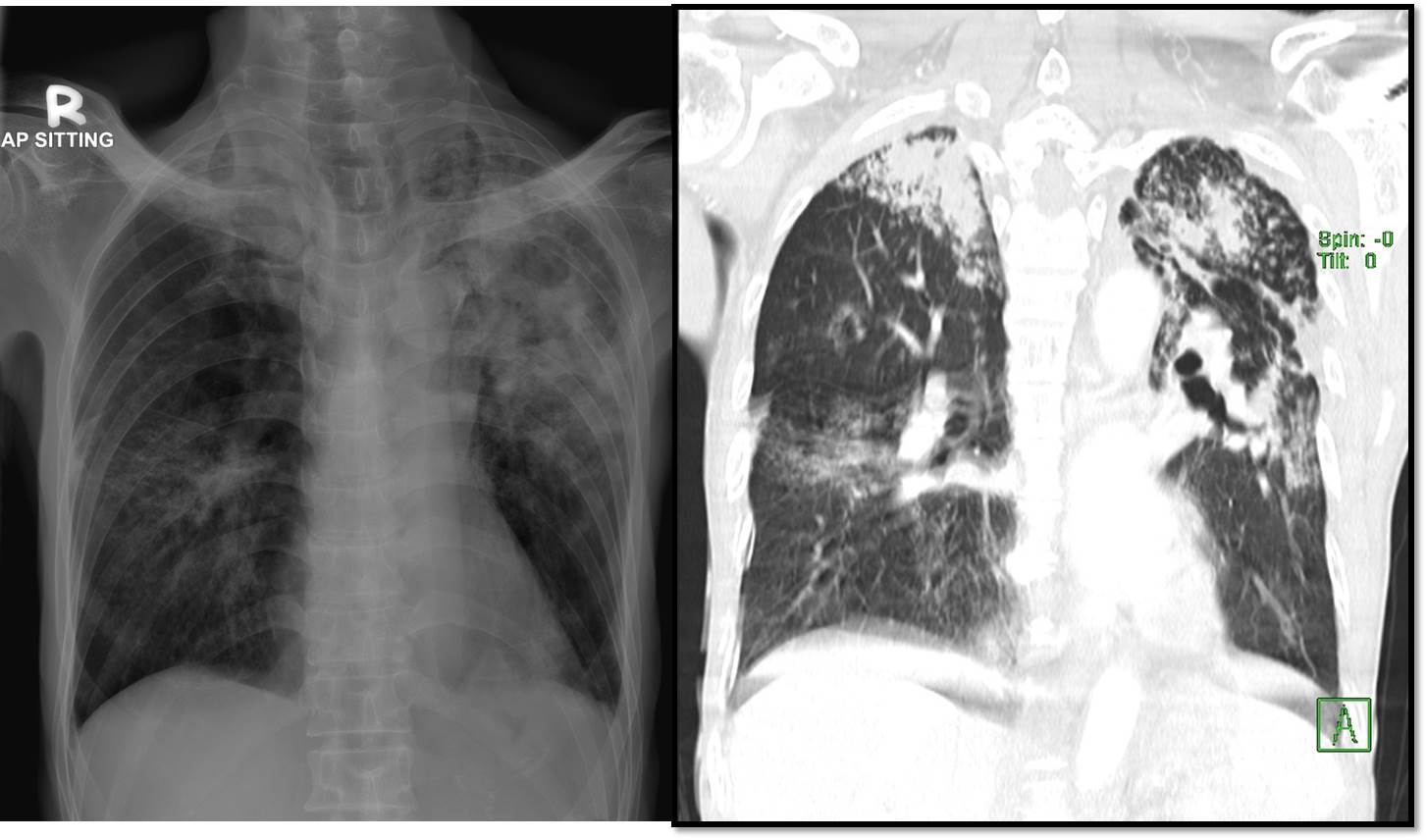
Radiographic findings:
- There are extensive consolidation and cavitating lesions seen at upper and midzone of the left lung (yellow arrow).
- Similar but less severe changes are also seen at right apical region (red arrow).
- Small reticulo-nodular opacities are also in the rest of the lungs.
- No mediastinal widening. No hilar mass.
- No cardiomegaly. No pleural effusion. No bone lesion.
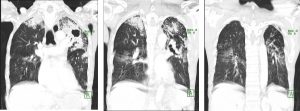
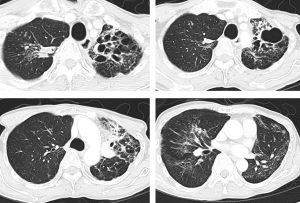
CT scan findings:
- There are multifocal collapsed-consolidations with cavitations seen predominantly involving both upper lobes, more severe on the left side.
- Multiple small lung nodules and tree in bud density are seen scattered in both lungs.
- Underlying chronic lung changes with fibrosis and emphysematous change are seen.
- The trachea and main bronchi appears ectatic. However no intraluminal lesion is seen.
- Subcentimeter paratracheal hilar and axillary nodes are seen.
- The heart is not enlarged. No pleural effusion is seen.
Diagnosis: Pulmonary tuberculosis (smear positive)
Discussion:
- Pulmonary tuberculosis (PTB) remains one of the major issue in our clinical practice.
- Due to population based vaccination, in many cases post primary tuberculosis is more common than primary tuberculosis.
- The most common radiographic finding of post-primary PTB is focal or patchy heterogeneous, poorly defined consolidation involving the apical and posterior segments of the upper lobes and the superior segments of the lower lobe.
- In the majority of cases, more than one pulmonary segment is involved.
- Cavitation is radiographically evident in 20–45% of patients, while air-fluid levels in the cavity occur in 10% of cases.
- Cavitation may progress to endobronchial spread and results in a typical ‘tree-in-bud’ distribution of nodules in addition to cavitation; this is considered a reliable marker of active TB.
- High-resolution CT is the method of choice to reveal tree-in-bud sign.
- Hilar or mediastinal lymphadenopathy is uncommon in post-primary PTB, seen in only 5–10% of patients.
- A pleural effusion is seen in approximately 18% of post-primary PTB.
Progress of patient:
- Patient was treated with anti-TB treatment.
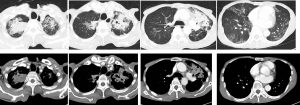
- Good response is seen clinically and radiologically.
- A repeat radiograph and CT scan shows resolving consolidation and cavitations with bronchiectatic change and fibrosis.