Case contribution: Dr Radhiana Hassan
Clinical:
- A 43 years old man
- No known medical illness
- Sudden onset of severe abdominal pain for one day, radiating to the back and relieves with patient bending forward
- No fever, no change in bowel habit, no vomitting
- Abdominal radiograph is unremarkable
- Serum amylase 2673, Hb 7.7 and TWBC 19.9
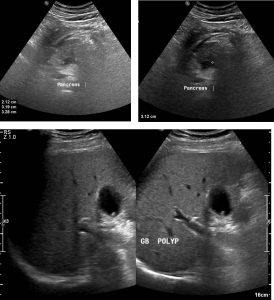
Ultrasound findings:
- The entire pancreas is enlarged measuring
- There is no calcification seen in the pancreas.
- No peripancreatic fluid collection or cyst is detected.
- The pancreatic duct is not dilated and no stone is detected in it.
- A small gall bladder polyp is seen. Liver is normal.
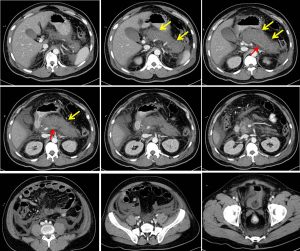
CT scan findings:
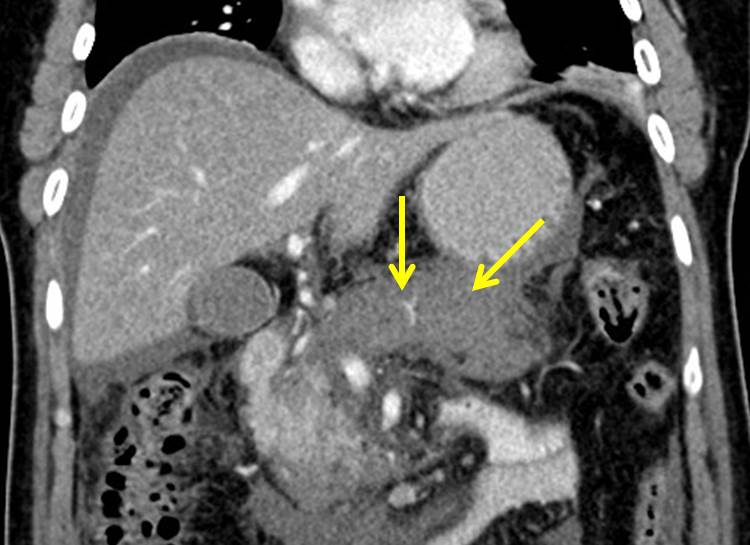
- The pancreas is enlarged and oedematous, appearing heterogeneously hypodense with irregular margin (yellow arrows).
- Generalised non-enhancement of the pancreas is seen. Only a small portion of normally enhancing pancreas is seen at the pancreatic head and uncinate process region.
- No pancreatic mass lesion detected.
- There is minimal peripancreatic fluid with marked peri-pancreatic fat streakiness.
- Irregular thickening of the Gerota and Zuckerkandl fascia are also observed bilaterally.
- Mild to moderate ascites noted with minimal interloop fluid observed.
- Non-enhancement of the splenic vein is noted from its insertion into the portal vein until near the splenic hilar region whereby some enhancement of the splenic vein is noted (red arrows).
Diagnosis: Necrotizing pancreatitis
Discussion:
- Acute pancreatitis is defined clinically as a disorder that includes abdominal pain (typically epigastric in location and radiating to the back) and serum amylase or lipase levels more than three times higher than normal.
- Acute necrotizing pancreatitis is a severe form of acute pancreatitis characterized by necrosis in and around the pancreas and is associated with high rates of morbidity and mortality.
- Imaging is not required for diagnosis in typical cases
- Imaging is performed
- to confirm the diagnosis of pancreatitis if symptoms are atypical or serum amylase or lipase levels are less than three times higher than normal,
- when the cause of pancreatitis is uncertain and an underlying neoplasm is suspected as a cause, and
- to confirm the diagnosis of necrosis when the patient’s condition does not improve or deteriorates
- Pancreatic necrosis may involves pancreatic parenchyma only, peripancreatic tissues only, or both pancreatic parenchyma and peripancreatic tissue (most common)
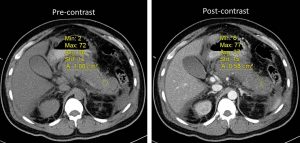
- On CT scan, pancreatic necrosis is suspected when any region of pancreatic parenchyma demonstrates no enhancement post contrast (an attenuation of less than 30 HU during the pancreatic parenchymal phase). Normal pancreatic parenchyma demonstrates maximum enhancement (typically, 100–150 HU); at approximately 40 seconds after intravenous contrast material administration.
- The severity of necrotizing pancreatitis at imaging is determined on the basis of the extent of parenchymal involvement by necrosis
- no necrosis= CT severity index 0
- <30% = CT severity index 2,
- 30%–50% = CT severity index 4 and
- >50% = CT severity index 6.
Reference:
- Necrotizing pancreatitis: diagnosis, imaging and intervention. RadioGraphics at https://doi.org/10.1148/rg.345130012
- Acute pancreatitis: The Radiology Assistant at https://radiologyassistant.nl/abdomen/pancreas/acute-pancreatitis
Recent Comments