Case contribution: Dr Radhiana Hassan
Clinical:
- A 70 years old lady
- No known medical illness
- Premormidly ADL independent
- Initially presented with dysphagia and treated as retropharyngeal abscess with IV antibiotic (CT scan done in another hospital)
- Took AOR discharge after started IV antibiotics for 2 days
- Came to our hospital due to persistent dysphagia
- On the day of admission to our centre noted patient is able to eat solid foods, afebrile
- FNPLS shows intact nasopharyns and vocal cord, fullness at left arythenoid, no mass seen.

Radiograph findings:
- There is pre-vertebral soft tissue thickening extending from C7 to the upper thoracic region (white arrow).
- Lucent areas are seen within which may represent air pockets (yellow arrow)
- Minimal mass effect to posterior wall of trachea with minimal narrowing.
- No adjacent bony erosion seen.
- Visualised lungs are normal.
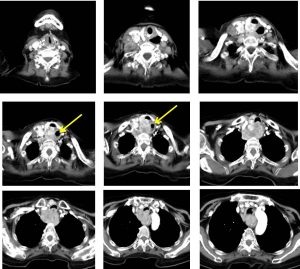
CT scan findings:
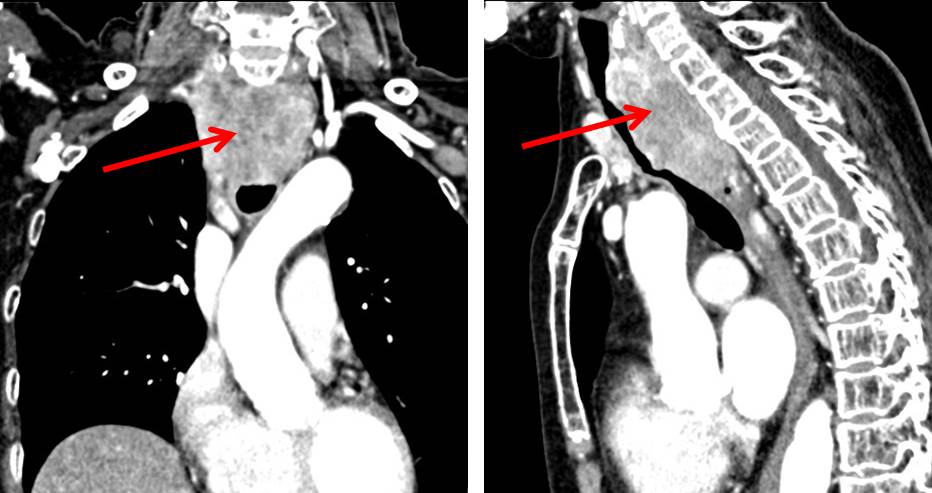
- There is lower anterior neck mass that extends from the level of C5 to T4 at the superior mediastinum.
- The mass shows heterogeneous enhancement following IV contrast.
- No clear plane is identified between this mass with the posterior aspect of the right thyroid gland.
- The posterior tracheal wall is compressed and flattened with irregular in outline that may represent infiltration.
- The tracheal lumen at this level is slightly narrowed.
- An air filled space is visualized on the left retropharyngeal space (yellow arrows) which could represent a dilated proximal oesophagus which is also displaced to the left
- The left thyroid gland, which is normal,
- Multiple enlarged lymph nodes are seen particularly on the right side.
- The right jugular vein is stretched anterior to the enlarged supraclavicular nodes but together with the rest of the great vessels of the neck they are patent and intact.
HPE findings:
- Macroscopy: specimen labelled as right cervical lymph nodes consistent with multiple pieces of greyish tissue measuring 24 mm in aggregate diameter
- Microscopy: section shows fragments of lymphoid tissue harboring malignant tumour arranged as papillary configuration, glands and islands. The cells are enlarged, round to ovoid in shape with clearing of the nuclei and nuclear overlapping. Occasional nuclear grooving and inclusion is seen. The cytoplasm is dense. There is no psammoma body seen.
- Immunohistochemical staining: the tumour cells are positive for CK7 and thyroglobulin, and negative for CK20
- Interpretation: right cervical lymph node: papillary thyroid carcinoma, neoplastic
Progress of patient:
- FNPLS shows no swelling or pus at posterior pharyngeal wall, left tonsil enlarged, piriform fossa clear bilaterally, no pooling of saliva at vallecula, vocal cord mobile, no phonatory gap
- OGDS done shows esophageal narrowing 20 cm from incisor, about 3 cm in length, normal mucosa, unable to pass through the narrowing of the esophagus, attempted for esophageal dilatation but abandoned.
- Complicated with nosocomial pneumonia during admission and succumb 3 months from initial presentation.
Discussion:
- Papillary thyroid carcinoma is the most common type of thyroid cancer.
- It is the 8th most common cancer among women and the most common cancer in women younger than 25 years old.
- Most patient presented before age of 40 years.
- Risk factors include radiation exposure and family history of thyroid cancer but majority of patients have no risk factors at all
- It is the cancer with the best prognosis and patient can be cured if treated appropriately and early enough
- Involvement of lymph nodes usually have almost no impact on survival and do not change the prognosis
- Most papillary thyroid cancers are asymptomatic. Most common symptom is a solitary palpable thyroid mass.
- It has a tendency to metastasize early to local lymph nodes (50%) compared to follicular thyroid cancer (10%). Usually lymph node metastasis is to ipsilateral jugular chain and confined to mid and lower lymph node levels III and level IV.
- Distal metastasis is less common with a prevalence of 5-10%.
- The best treatment for papillary thyroid cancer is almost always total thyroidectomy.
- Why total thyroidectomy?
- Most papillary thyroid carcinomas are multifocal,
- post operative radioiodine ablation therapy is more effective without thyroid tissue to soak up the radiation,
- more accurate follow up thyroglobulin test for recurrence and
- recurrent rate lower than after a lobectomy
Recent Comments