Case contribution: Dr Radhiana Hassan
Clinical:
- A 60 years old lady
- No known medical illness and no history of trauma
- Presented with back pain for 2 weeks. No fever.
- Clinically power and sensation is reduced.
- Imaging was done to rule out spinal stenosis
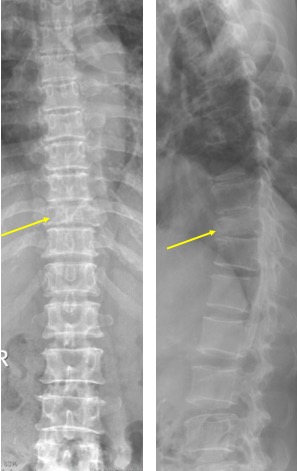
X-ray findings:
- Reduced T10 vertebra body height (yellow arrows) in keeping with compression fracture.
- Suspicious retropulsed bony segment. Pedicle is still intact.
- The rest of the vertebra bodies height are normal.
- No obvious soft tissue mass seen
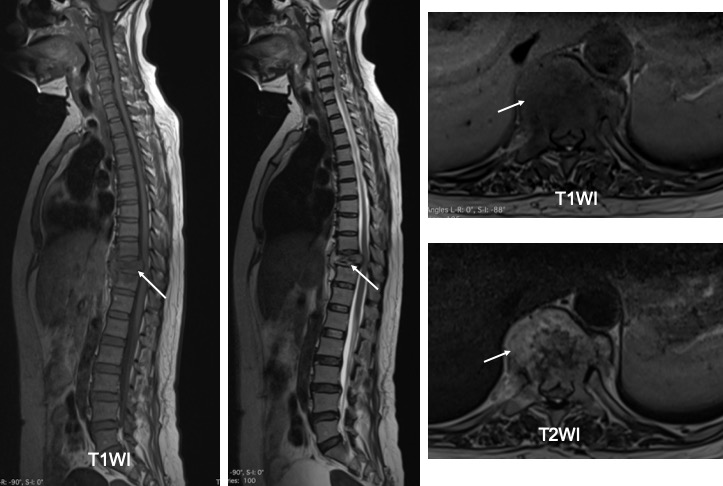
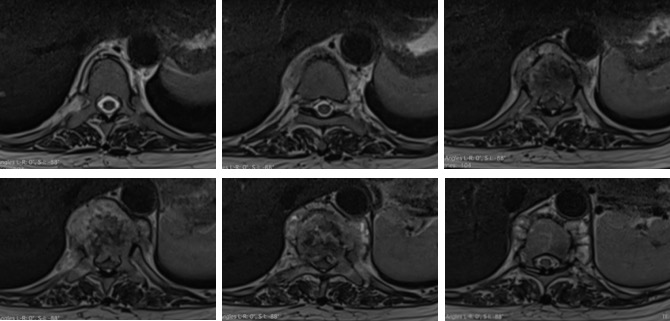
MRi findings:
- There is compression fracture of T10 (white arrows) with retro pulsed fragment causing compression onto the spinal cord.
- The cord shows high signal intensity at this place suggestive of cord edema.
- There is a soft tissue collection around the crushed body of T10. There are subligamentous extentions of this collection.
- It is confined by the anterior longitudinal ligament anteriorly. It extends superiorly to the level of lower end plate of T8 and inferiorly to the lower endplate of L1.
- The visualised brain and craniocervical junction are normal.
Progress of patient:
- MTB PCR was positive
- Patient was started on anti-TB
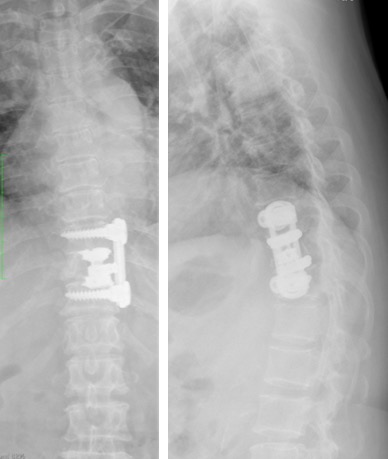
- Patient also had surgical instrumentation and stabilisation of the compression fracture
Diagnosis: Spinal tuberculosis
Discussion:
- Thoracic spine is the most common extrapulmonary spinal site for TB.
- 5% of all TB patients have spine involvement
- Early infection shows metaphysis involvement with subligamentous spread to contiguous multilevel or skip noncontiguous segment (15%)
- Paraspineal abscess formation occurs in about 50% of cases and usually anterior location (more common than in pyogenic infection)
- Initial stage does not involve disc space (also distinguishing feature of pyogenic osteomyelitis)
- Chronic infection can cause severe kyphosis. Risk factors for buckling collapsed include retropulsion, subluxation, lateral translation and toppling changes.
- Pharmacological treatment with antiTB (RHZE for 2 months then RH for 9-18 months)
- Operative approach such as anterior decompression, strut grafting with or without posterior instrumented stabilization, posterior column shortening, bone grafting, pedicle subtraction osteotomy or direct decompression /internal kyphectomy
- Complications: kyphosis/gibbus deformity, TB arteritis/pseudoaneurysm, sinus formation and Pott’s paraplegia (spinal cord injury caused by abscess/bony sequestra or meningomyelitis

Recent Comments