Case contribution: Dr Radhiana Hassan
Clinical:
- A 37 years old female with no previous medical illness
- Presented with persistent headache at bitemporal and occipital region
- Associated with blurred vision for the past one week
- Vomiting 2-3 times per day
- Clinical examination: GCS 15/15. No neurological deficit.
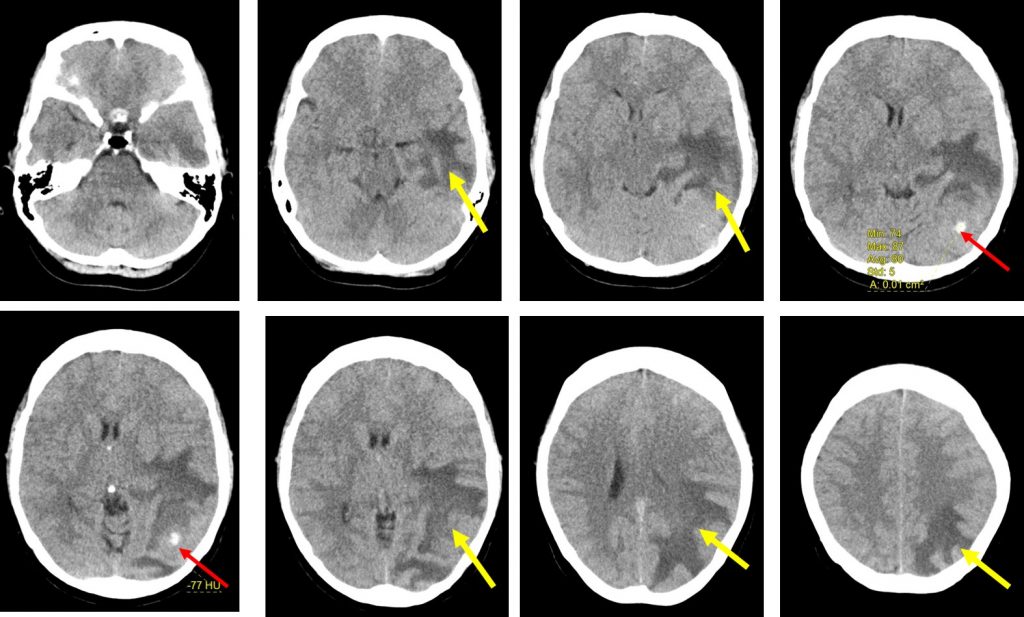
CT scan findings:
- There is a hyperdense lesion (HU 75-85) seen at the left occipital region (red arrows) likely of haemorrhage.
- A vague lesion seen surrounding the bleed measuring 4.0 cm x 2.7 cm x 3.4 cm (AP x W x CC)
- Associated extensive white matter oedema at left parieto-occipito-temporal lobe (yellow arrows).
- It causes mass effect and compressing on the left lateral ventricle.
- The adjacent sulci are also effaced and mild midline shift to the right.
- The rest of the grey and white matter differentiation is preserved.
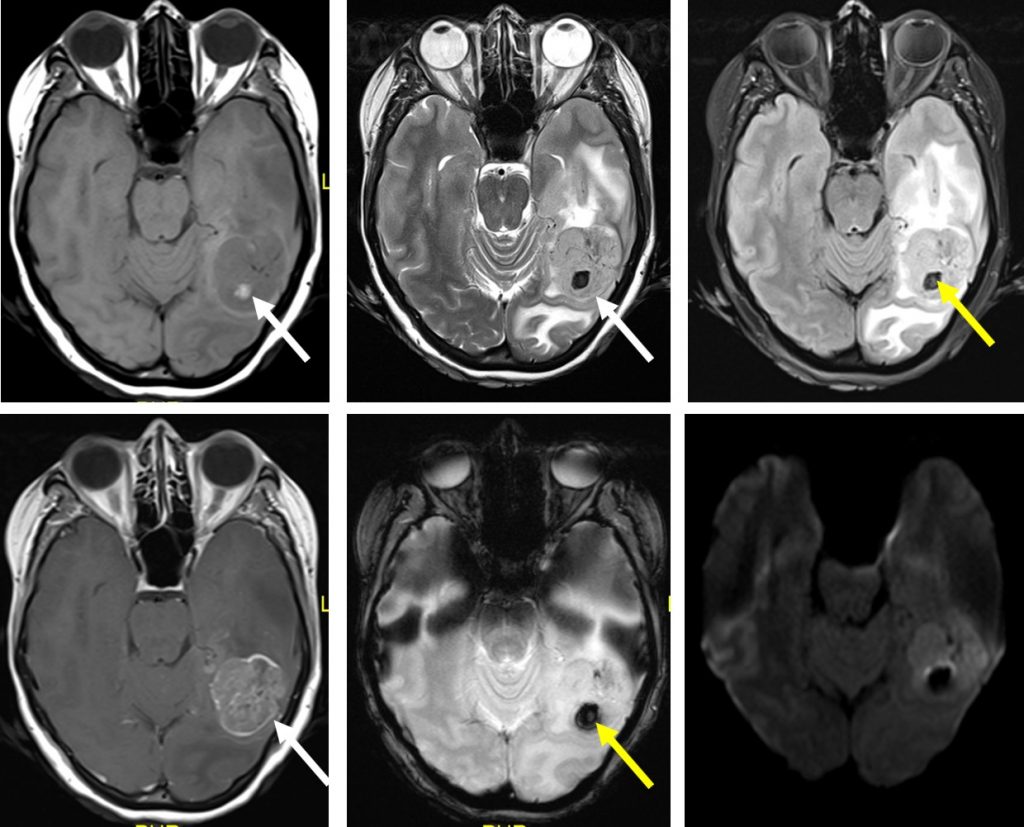
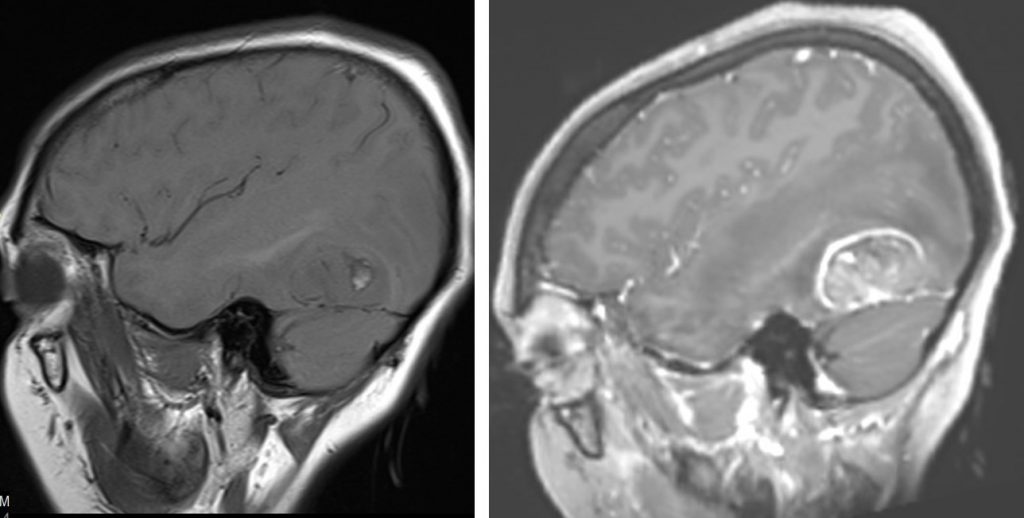
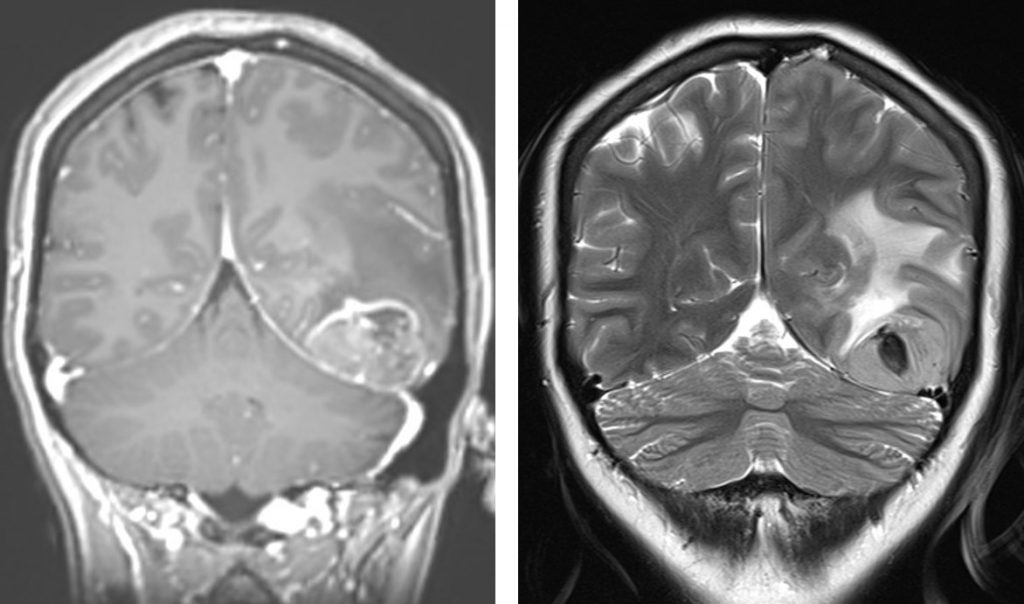
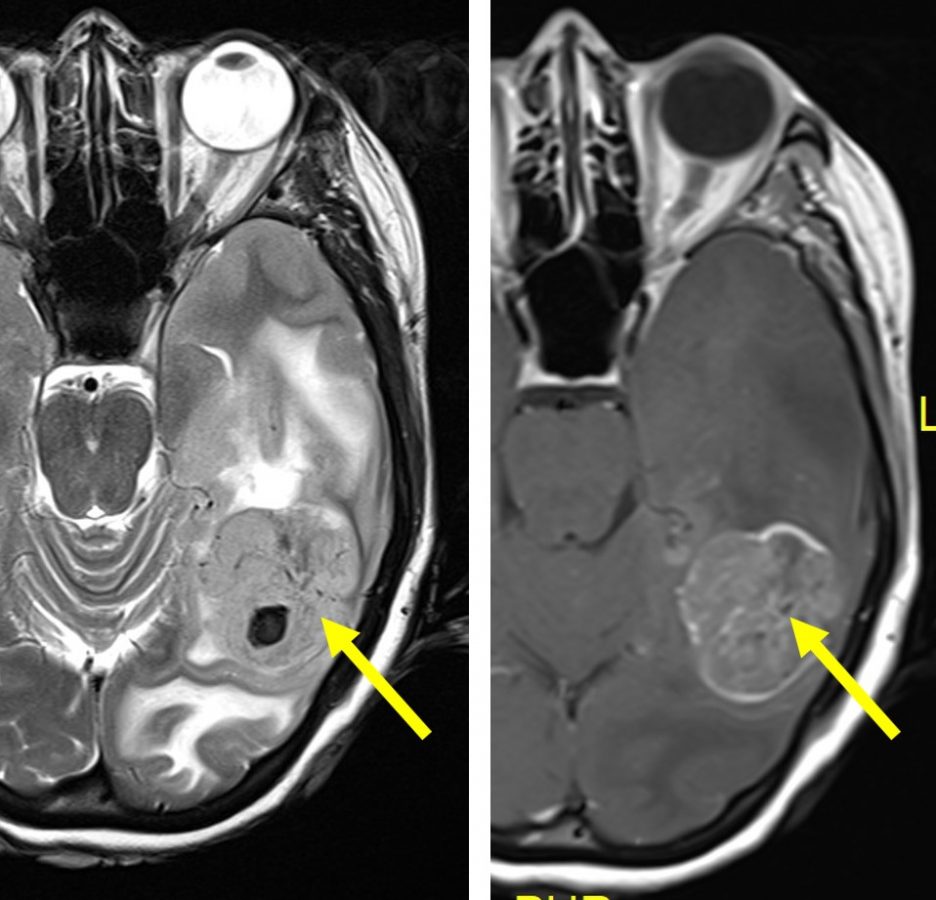
MRI findings:
- There is a solitary lobulated intra-axial mass seen within left occipital lobe.
- It is hypointense on T1, hyperintense on T2/FLAIR with heterogenous mainly peripheral enhancement post contrast.
- Intralesional subacute haemorrhage is seen, evidence by hyperintense signal on T1, hypointense signal on T2 with blooming artefact on GRE/SWI sequence.
- Minimal restricted on DWI/ADC sequence.
- Associated marked perilesional oedema is noted, causing effacement of the adjacent temporo-parieto-occipital sulci and ipsilateral lateral ventricle. Minimal midline shift to the right is observed, measures about 0.2cm.
- The contralateral lateral ventricle, third and fourth ventricles are not dilated.
- No subfalcine herniation. No abnormal meningeal enhancement.
Progress of patient:
- Underwent left craniotomy and tumour excision
- Discharged well with phenytoin
- Had radiotherapy
- Developed drug reaction with popular rash over hand, forearm and face.
- Also noted to have transaminitis and eosinophilia.
- Also had complication of hospital acquired pneumonia
- Patient succumb 4 months after diagnosis
HPE findings:
- Macroscopy: specimen labelled as brain tumour, consists of multiple pieces of tan greyish tissue measuring 17 mm in aggregate diameter.
- Microscopy: section shows fragment of tumour tissues composed of diffusely sheets of cellular tumour. The tumouor cells displays moderate to marked pleomorphic, hyperchromatic to vesicular nuclei with some shows prominent nucleoli. Mitosis are seen (10-11 per 10hpf). In areas, multinucleated tumour cells are also present. There are no necrosis or microvascular proliferation are noted in this biopsy.
- Immunohistochemistry of tumour cells: GFAP positive, CKAE1/AE3 negative and Ki 67 proliferation index 10%
- Interpretation: Anaplastic astrocytoma WHO Grade III
Diagnosis: Anaplastic astrocytoma
Discussion:
- Anaplastic astrocytoma is a diffusely infiltrating malignant astrocytoma with anaplasia and marked proliferative potential
- Neoplastic cells almost always found beyond areas of abnormal signal intensity
- It may involve and expand the overlying cortex
- Location: hemispheric white matter in frontal and temporal lobes. Less commonly seen in brain stem and spinal cord
- On imaging it predominantly involve the white matter with variable enhancement, may appear well circumscribed, usually no enhancement, less common feature is focal, nodular or patchy enhancement. Ring enhancement raised suspicious of glioblastoma
- CT scan shows low density mass, calcification and hemorrhage are rare
- T1WI- iso to hypointense to WM, calcification and hemorrhage are rare, may expand the cortex
- T2WI-heterogeneously hyperintense, may appear discrete but infiltrate adjacent brain, rarely prominent flow voids are present suggesting progression to glioblastoma
- FLAIR-heterogeneously hyperintense
- DWI-no restricted diffusion
- T1+Contrast-usually no enhancement
- MRS-elevated Cho/Cr ration, decreased NAA
- MR perfusion-elevated maximum rCBV compared to low grade glioma