Case contribution: Prof. Dr Azian Abd Aziz
Clinical:
- A 4 years old boy who was previously born via emergency caesarean section for fetal distress.
- He is being followed-up for global developmental delay.
MRI findings:
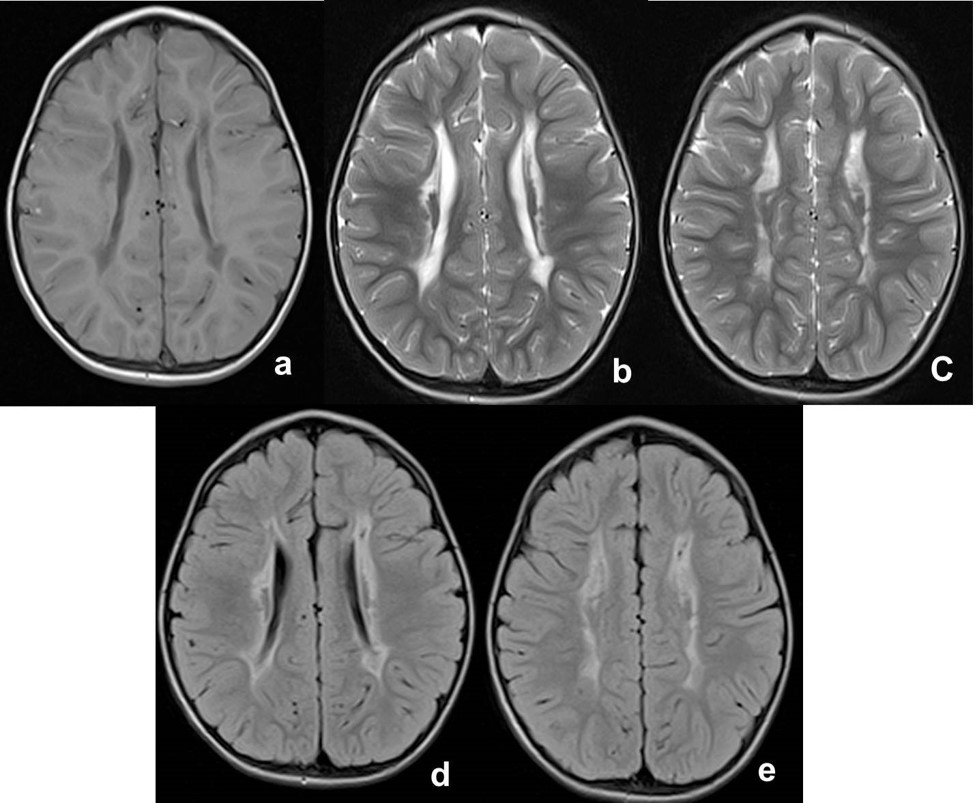
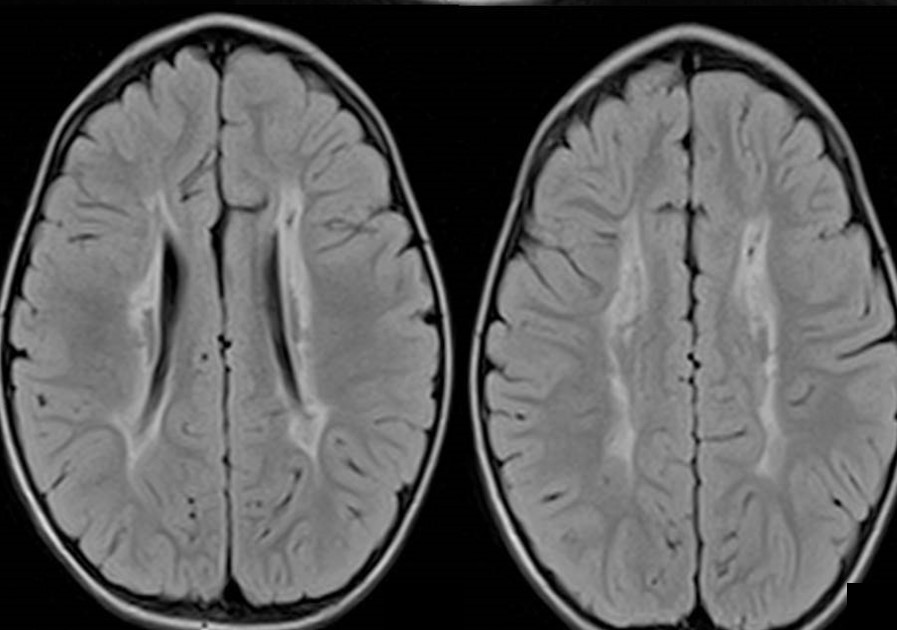
- Axial MRI brain show almost symmetrical bilateral periventricular hyperintense T2 and FLAIR signal (Figs. b-e), which is hypointense on T1 (Fig. a).
- The ventricles are not dilated and no other abnormality is detected.
Diagnosis: Bilateral periventricular leukomalacia (PVL).
Discussion:
- PVL is a white matter damage following hypoxic-ischemic injury that consist of periventricular focal necrosis, resulting in cystic formation and diffuse cerebral white matter injury.
- PVL is the major form of cerebral white matter injury that affects premature infants.
- The brain of premature infants is more vulnerable to hypoxic ischemic insults because of incomplete development of vessels that supply the area near the ventricles, due to impaired cerebral vascular autoregulation and vasoconstriction and also due to cellular factors during the period of development.
- Ultrasound is commonly used as the initial standard investigation because it is portable and least expensive but it has limited sensitivity and specificity to detect PVL, especially if the lesions are less than 0.5 cm.
- MRI has the advantage in which increased signal intensity on T2 weighted imaging highlights areas of presumed gliosis. Once myelination has occurred, the fluid attenuated inversion recovery (FLAIR) sequence is particularly useful for demonstrating periventricular and cortical gliosis. The low signal of CSF with the high signal of most parenchymal pathology, enhances the detection of lesions adjacent to CSF spaces.
- Published literature has demonstrated that pre-term infants with PVL have reduced cortical grey matter volumes, which suggest that PVL has an impact on cerebral cortical development, which may explain the cognitive deficits associated with this condition.
Recent Comments