Clinical:
- A 59 years old man
- Underlying DM, HPT and hyperuricaemia
- Alleged fall at home, missed steps and landed backward
- No loss of consciousness, no vomiting, no headache, no blurred vision
- Complaint of scalp swelling at left temporoparietal region
- Examination showed GCS 15/15, no neurological deficit
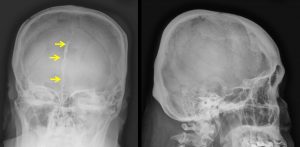
- Skull radiograph showed no depressed skull fracture
- Patient was discharged home
- Presented again after 2 days with severe headache and vomiting
Radiographic finding:
- Skull radiograph do not demonstrate any fracture line.
- An incidental finding of calcification, most probably falx calcification
- No obvious soft tissue haemotoma
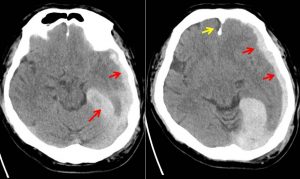
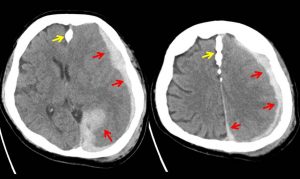
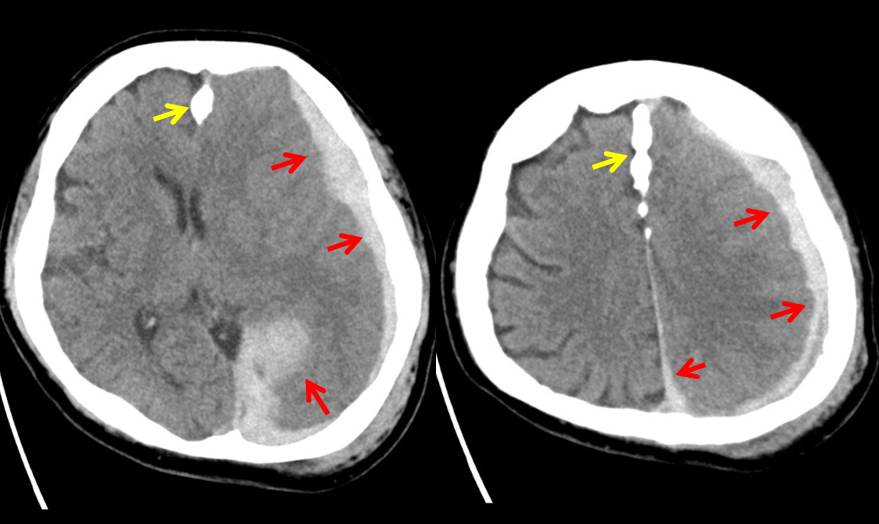
CT findings:
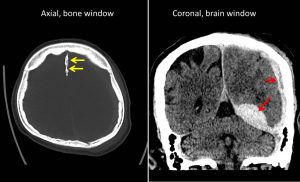
- Urgent non-contrast CT brain done
- Acute subdural haemorrhage (red arrows) is seen at left cerebral hemisphere causing compression to the underlying brain parenchyma, particularly at the left temporal -parietal lobe.
- It extends to left interhemispheric fissure and left tentorium
- It has the maximum thickness of 2.0 cm at left tentorium.
- It is associated with effacement of the adjacent sulci and right lateral ventricle. Poor grey white matter junction differentiation of the left cerebral hemisphere in keeping with cerebral oedema
- There is about 1.1 cm midline shift to the left.
- Prominent temporal horn of the left lateral ventricle noted, in keeping with obstructive hydrocephalus.
- No skull fracture. Falx calfication (yellow arrows) as noted on skull radiograph
- Scalp hematoma at left parieto-occipital region.
Diagnosis: Acute left subdural haemorrhage
Discussion:
- Subdural haemorrhage is accumulation of blood in potential space between pia-arachnoid membrane with dura mater
- Elderly patient is predisposed to this type of injury due to longer bridging veins in senile brain atrophy
- No consistent relationship with skull fracture
- CT scan shows crescent-shaped hyperdensity at cerebral convexity with frequent extension to interhemispheric fissure and along tentorial margins
- Haematoma freely extending across suture lines, but do not cross midline
- Can be bilateral in 15-25% (adults) and 80-85% (infants)
- Mortality rate 35-50% due to various associated injuries
Progress of patient:
- Patient deteriorated with drop in GCS
- Left decompressive craniectomy with duroplasty performed
- Develop new onset AF
- Septic shock secondary to pneumonia
- Died 8 days after admission