Case scenario:
- A 40 years old lady, no known medical illness
- Recently involved in MVA, preceded with right upper limb rigidity
- Had antegrade amnesia post trauma
- MRI done shows space occupying lesion in parietal lobe
- Referred to our centre for excision of tumour
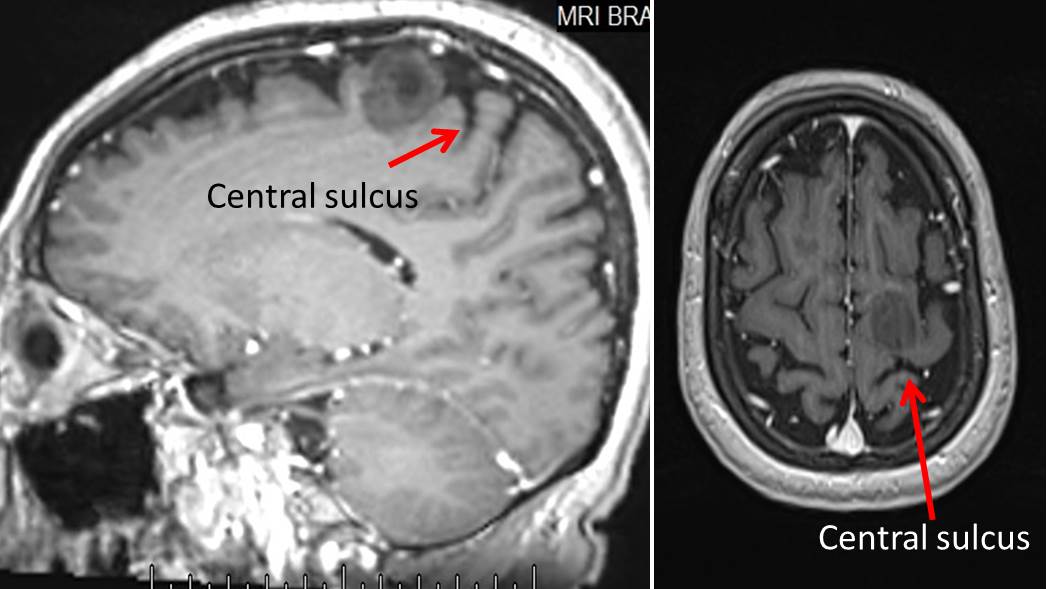
Issue raised by neurosurgeon: Where is the lesion? In frontal or parietal lobe? Neurosurgeon needs to know exact location to consider the risk of operation.
The key to answer the question is by identifying central sulcus. Central sulcus in a very important landmark that separate the frontal lobe from parietal lobe. It separate the precentral gyrus (motor cortex) from post central gyrus (sensory cortex). A few signs/ways to recognize central sulcus has been described. It is important to note that not all signs present in any one patient.
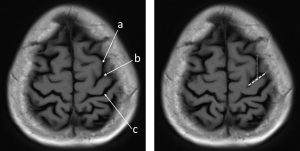
1) Upper T sign
- Using axial image ( I am using MRI of other patient since this patient do not demonstrate this sign)
- a: Find superior frontal sulcus, at the top axial slice it runs parallel to interhemispheric fissure.
- b: the precentral sulcus intersect superior frontal sulcus in a “T” junction
- C: The central sulcus is next to posterior sulcus
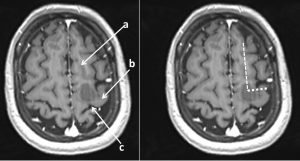
2) L sign
- Using axial scan (using MRI of this patient)
- a: Find superior frontal gyrus, at the top axial slice it runs parallel to interhemispheric fissure.
- b: It intersect precentral gyrus in an “L” junction
- C: The central sulcus is immediately posterior
3) Lower T sign
- Using axial image (using MRI of another patient)
- a:locate the inferior frontal sulcus
- b: It terminates posteriorly in the precentral sulcus in a T junction
- c: The central sulcus is the next posterior sulcus
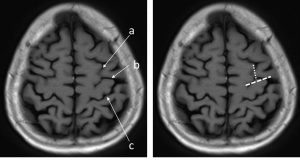
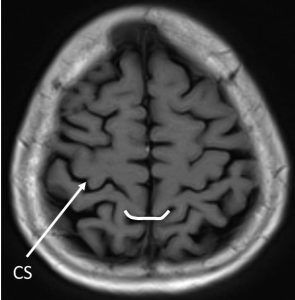
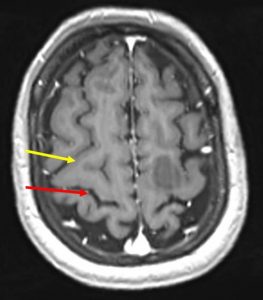
4) Bracket sign
- The marginal sulcus is visible immediately posterior to the central sulcus
- The paired pars marginalis form a ‘bracket’ to each side of the interhemispheric fissure
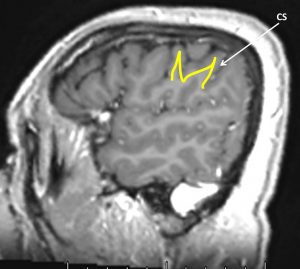
5) M sign
- Using sagittal view ( I found this sign is not easy to locate)
- The inferior frontal gyrus has a characteristic “M” configuration and terminates posteriorly in the precentral gyrus.
- The central sulcus is immediately posterior
6) Midline sulcus sign
- The longest and most prominent convexity sulcus that reaches the midline interhemispheric fissure is the central sulcus
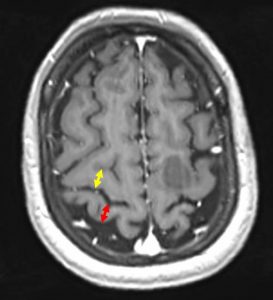
7) Thin postcentral gyrus sign
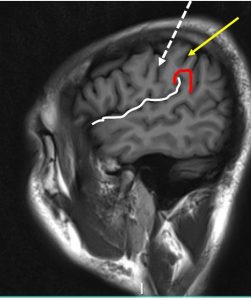
- The post central gyrus (red arrow) is thinner than the precentral gyrus (yellow arrow)
8) Sigmoidal hook (handknob/omega) sign
- The precentral gyrus bulges posterior at the hand motor area
- Note the different configuration of the bulges, thus the different name sign
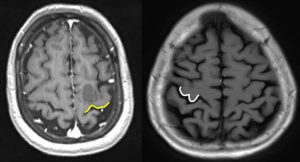
9) Bifid post central gyrus
- The post central gyrus is split medially by the pars marginalis (yellow arrow) of the cingulate gyrus
10) Gray white matter sign
- The differentiation of gray white matter around the central sulcus (red arrow) is reduced compared to precentral (yellow arrow) and postcentral gyrus on T1WI
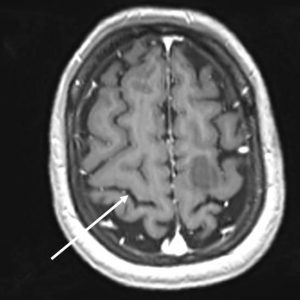
11) Using lateral sagittal images:
- Identify the sylvian fissure (white line)
- Follow the sylvian fissure posteriorly
- The posterior end is cupped by the supramarginal gyrus of the parietal lobe (red line)
- The sulcus at the anterior border of the supramarginal gyrus is the postcentral sulcus (yellow arrow)
- The sulcus in front of it is the central sulcus (white arrow)
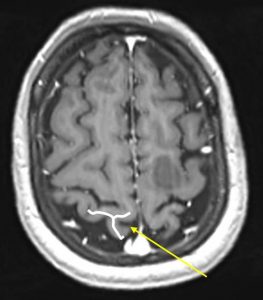
12) Using midsagittal image
- a: Identify corpus callosum
- b: Identify the cingulate gyrus and sulcus (red line)
- c: Follow the cingulate sulcus posteriorly and superiorly. This is the marginal branch (yellow line)
- d: First sulcus in front of the marginal branch is the central sulcus (white arrow)
- Second image shows the location of central sulcus (white arrow) in our patient
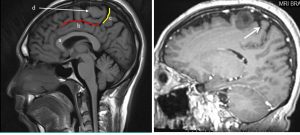
So, as a conclusion the mass lesion seen in our patient is located within the precentral gyrus, not in parietal as initially reported.
Progress of patient: Biopsy was done, unevetful procedure.
HPE findings:
- Macroscopy: specimen labelled as brain tumour consist of whitish and reddish tissue
- Microscopy: levels show a fragment of lesional tissue exhibiting moderate increase in cellularity and nuclear atypia in a fibrillary background. There is no mitosis seen. No area of necrosis or microvascular proliferation identified.
- Immunohistochemical staining:GFAP: positive, Ki67: Low (<1%).
- Interpretation: Low grade glioma in favour of diffuse astrocytoma, WHO grade II