Clinical:
- A 63-year old with underlying HPT and DM
- Presented with altered sensorium.
- He had a fall 3 days prior to the presentation.
CT scan findings:
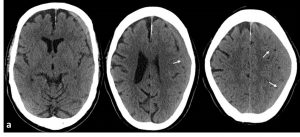
- Axial non-contrasted CT scan of the brain on admission (a) shows a crescent-shaped collection in the left cerebral convexity (arrows) of the fronto-parietal region.
- The collection is isodense compared to brain parenchyma.
- It crossed the suture but not crossing the midline.
- There is compression of the underlying brain with effacement of the cerebral sulci.
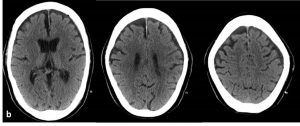
- A repeat non-contrasted CT scan post operation (b) shows no more collection in the left subdural space with minimal air pockets secondary to changes of the surgical procedure.
Diagnosis: Subacute subdural hemorrhage.
Discussion:
- A subdural hemorrhage is a collection of blood below the inner layer of the dura but external to the brain and arachnoid membrane.
- Generally, acute subdural hemorrhages are less than 72 hours old and are hyperdense compared with the brain parenchyma on CT scan.
- The subacute phase begins 3-7 days after the injury up to 3 weeks duration. At this time it is usually isodense to brain parenchyma as illustrated in this case.
- Chronic subdural hemorrhages develop over the course of weeks and are hypodense compared with the brain.
- Mixed density occurs when acute bleed has occurred into a chronic subdural hemorrhage.
- The classic appearance of subdural hemorrhage is described as a crescent-shaped extra-axial collection that spreads diffusely over the affected hemisphere. The density depends on age of hemorrhage.
- Subacute hemorrhage may become isodense to adjacent cortex making identification potentially difficult. In these cases, contrast enhanced CT scan or MRI is often useful.
