Clinical:
- A 26 years old injury
- Alleged sports injury
- Abdominal pain and persistent vomiting after collision with colleague during a futsal game.
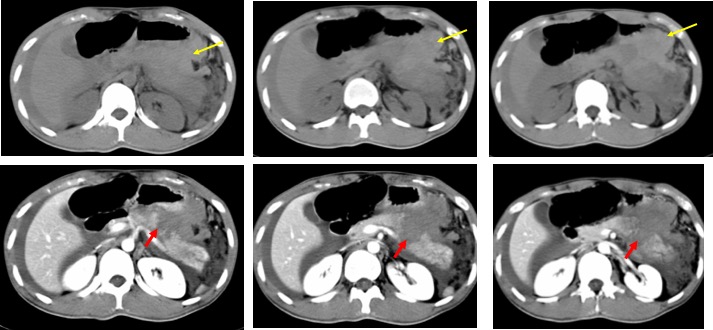
CT scan findings:
- A linear hypodensity at body of pancreas (red arrows) in keeping with laceration
- Separation of proximal and distal part of the pancreas
- Associated with surrounding hyperdense collection (yellow arrow)
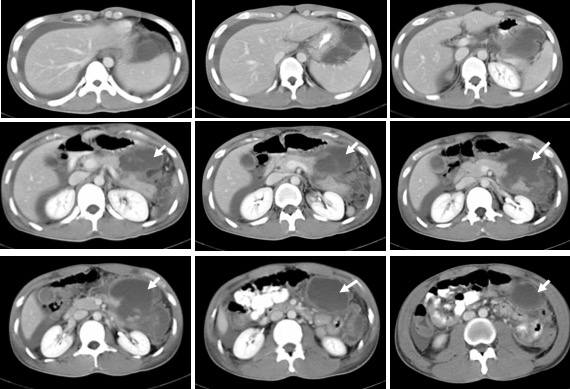
CT scan done 3 days after initial CT:
- The previously seen laceration at body of pancreas is better demonstrated.
- There is collection seen extending from this region into the lesser sac (white arrows).
- The collection is multiloculated, hypodense and show wall enhancement post contrast
- No evidence of vascular injury.
- Splenic and portal veins are normal.
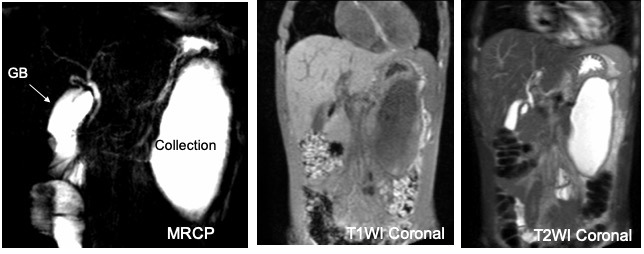
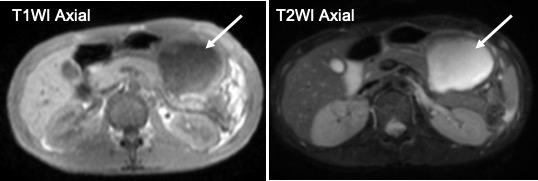
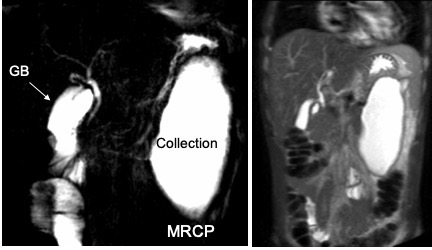
MRI and MRCP done 2 weeks later:
- The previously seen collection adjacent to pancreatic laceration is still seen
- No dilated intrahepatic duct or biliary tree or pancreatic duct
Diagnosis: Traumatic pancreatic pseudocyst.
Discussion:
- Trauma to the pancreas constitutes 2% of all abdominal injuries.
- One-third of pancreatic injuries are due to blunt injury.
- Pancreatic injuries are associated with high mortality rate.
- Complications of the injury including pancreatic abscess, fistulae, hemorrhage or pseudocyst.
- Trauma is an etiological factor in 3-8% of adult pancreatic pseudocyst cases, but it is responsible for almost all pediatric pancreatic pseudocysts.
- Pancreatic pseudocyst is a localized collection of pancreatic secretions lacking an epithelial lining as a result of pancreatic inflammation or ductal disruption.
- It is seen on imaging as fluid-filled oval or round collections with a relatively thick wall.
- They can be multiple and are most commonly located in the pancreatic bed. However, they can be found anywhere from the groin to the mediastinum and even in the neck.
- Although pancreatic pseudocyst may regress on its own and requires no further treatment, interventions are required in selected cases
- Those complicated with infections, large size causing mass effect symptoms such as gastric outlet obstruction, bowel obstruction, hydronephrosis and biliary obstruction, diameter increasing in size or greater than 5 cm, recurrence following previous resection or aspiration, and persistent symptoms may be treated with open surgical intervention, percutaneous or endoscopic drainage of collection.
Progress of patient:
- Patient was managed non-operatively
- He was discharged 17 days after admission
- Recovered well