Case contribution: Dr Radhiana Hassan
Clinical:
- A 38 years old man
- No known medical illness
- Presented with headache, nausea and vomiting for one week. No fever. No history of trauma.
- Clinical examination was unremarkable
- Imaging done in another hospital reported as brain tumour
- Initial blood investigation shows leukocytosis
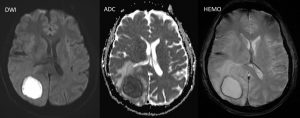
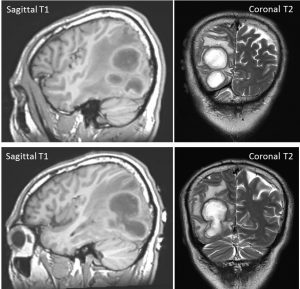
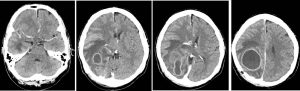
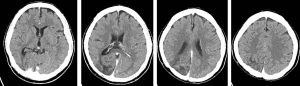
MRI findings:
- Limited sequences for preoperative assessment performed as examination already done in another hospital before recently.
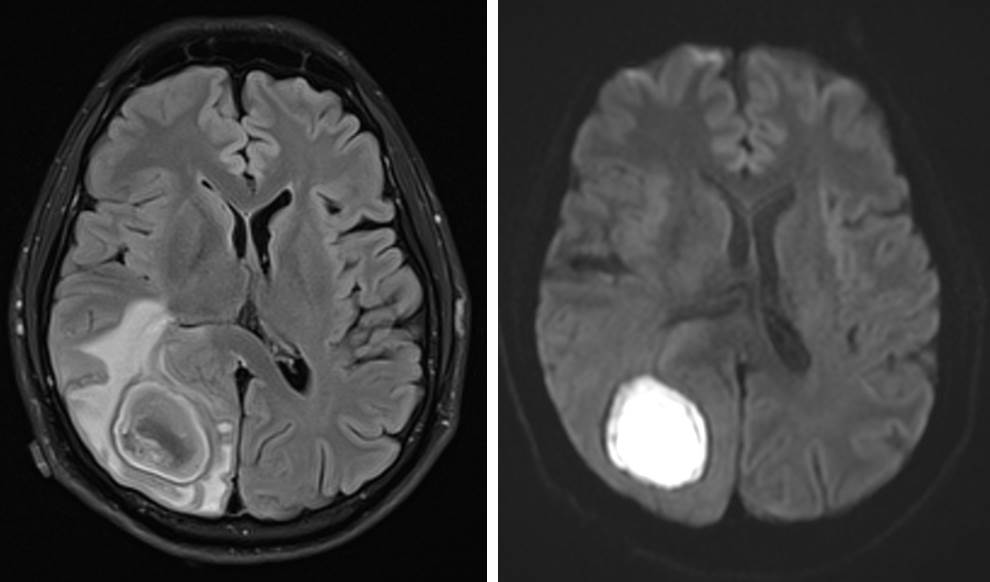
- There is a large multilobulated intra-axial mass lesion at right temporo-parieto-occipital region, measuring about 3.7 x 3.0 x 4.7 cm (AP x W x CC).
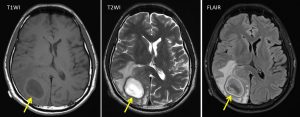
- It is heterogenously hypointense in T1 sequence and hyperintense in T2 sequence – and partially restricted on FLAIR acquisition.
- Restricted diffusion is also observed on DWI/ADC sequences.
- Presence of marked vasogenic perilesional white matter oedema is also seen.
Diagnosis: Cerebral abscesses.
Discussion:
- Cerebral abscesses are an uncommon but potentially life-threatening intracranial infection.
- The incidence is 0.4 to 0.9 cases per 100,000 people.
- Classic MR imaging findings of abscess include a contrast-enhanced rim that is T1 isointense to hyperintense relative to white matter and T2 hypointense surrounding a necrotic center. Characteristic peripheral T1 and T2 signal shortening may be due to collagen, hemorrhage, or free radical.
- Thinning of the capsule on the white matter side of the abscess, a finding due to relative hypovas-cularity in this region, is thought to relate to the propensity of abscess to decompress into the ven-tricles in advanced stages of disease
- It shows characteristic hyperintensity on DW images and corresponding hypointensity on ADC maps; however, these findings were not always pathognomonic for abscess
- At conventional MR imaging, the major differential diagnosis for abscess is cystic or necrotic tumor. These two entities can be differentiated using DW imaging.
- In addition to their use in differentiating infectious from noninfectious brain masses, DW imaging characteristics can be used to distinguish etiologic agents of abscess. Reduced diffusion is a fairly consistent finding among pyogenic and fungal abscesses. Whereas, parasitic infection with Toxoplasma gondii demonstrates increased diffusivity.
- MR spectroscopy is also helpful in these cases. The spectral signature of abscess includes elevated acetate, succinate, lactate, and alanine signals. Amino acids from neutrophil-driven protein breakdown are specific for pyogenic abscess.
Progress of patient:
- Craniotomy and pus aspiration done (about 43 cc pus aspirated)
- Pus sent for culture and sensitvity for fungal, TB and bacterial are all negative.
- Culture of toxoplasmosis also negative
- Patient recovered well