Case contribution: Dr Radhiana Hassan
Clinical:
- A 40 years old female
- Underlying connective tissue disease on medication
- Presented with headache, worsening in a few days
- No fever, no meningism and no symptom of increased intracranial pressure
- No body weakness
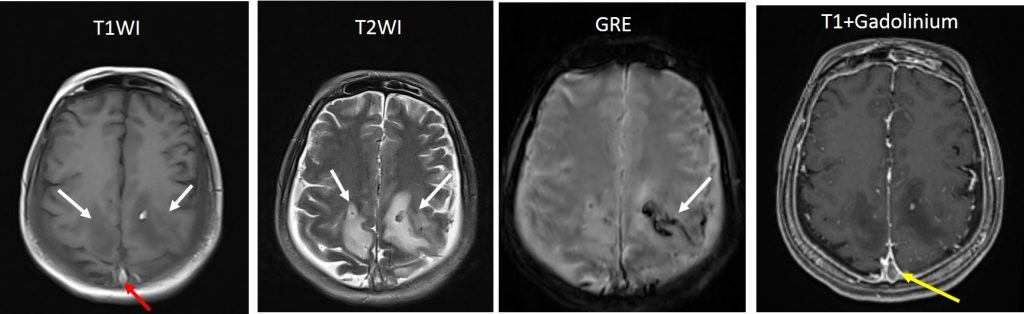
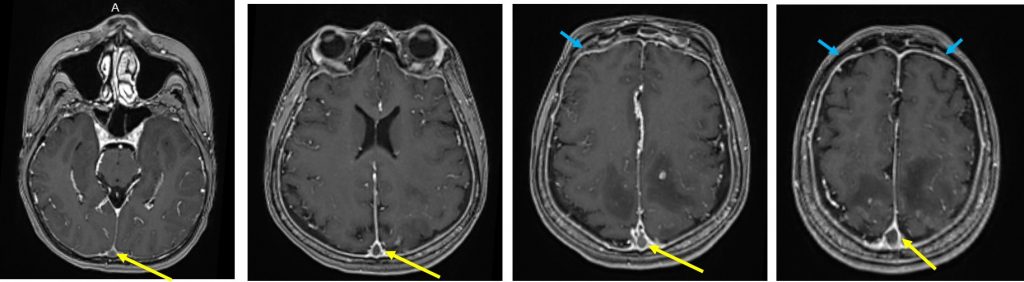
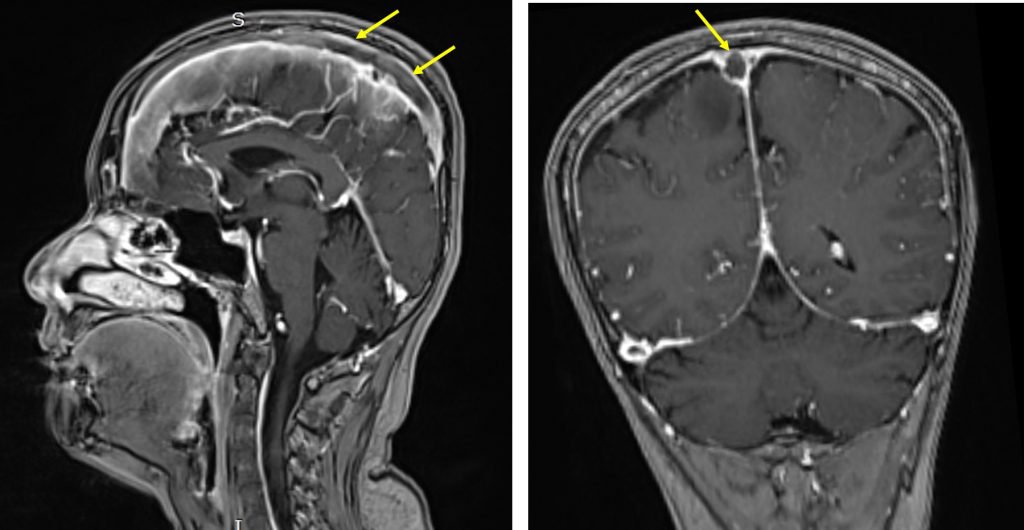
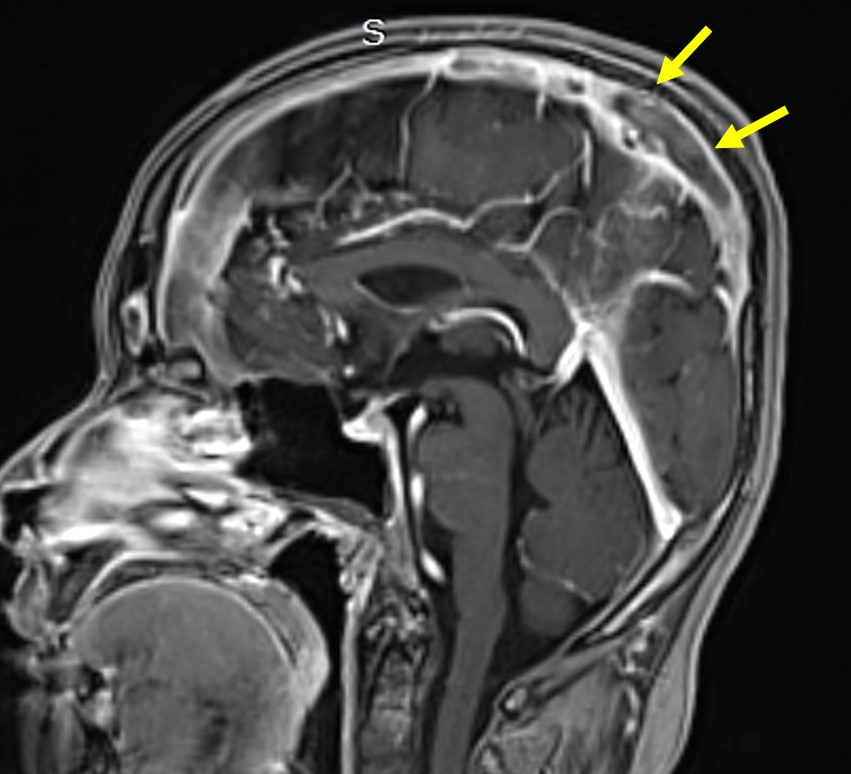
MRI findings:
- Venous infarction with hemorrhagic component seen at both parieto-occipital region (white arrows).
- Subacute blood clot seen within the superior sagittal sinus extending (red arrow) to confluent and right transverse sinus (images not shown)
- Post contrast shows filling defect within the sinuses mentioned above (yellow arrows)
- Abnormal generalised dural enhancement is also seen
Diagnosis: Cerebral venous thrombosis complicated by hemorrhagic venous infarction.
Discussion:
- Cerebral venous thrombosis refers to thrombus formation in either the deep or superficial venous drainage of the brain.
- It prevents normal drainage causes break of blood brain barried and leak of blood into the brain tissue
- It is a rare condition and aetiology is multifactorial.
- About 30-40% of patients presented with intracranial hemorrhage. Bilateral parenchymal hemorrhage with clinical evidence of hypercoagulable state should raised suspicion of this condition.
- Isolated subarachnoid hemorrhage may also occur although rare incidence.
- Non-contrast CT shows hyperdensity of a cortical vein or dural sinuses. Acutely thrombosed veins appear as homogenous hyperdensity that fills veins and sinuses. This sign is seen in about one third of patient
- Post contrast CT may show fillind defect (delta sign, dense triangle sign). It may also shows enhancement of dural lining of the sinus.
- An ischaemic infarction with hemorrhagic component may also be seen.
- MRI show thrombus with variable signal depending on age of the thrombus.