Case contribution: Dr Radhiana Hassan
Clinical:
- A 52 years old male
- No known medical illness
- Presented with lower back pain more on the right side for one wee, continuous and worsening, pain score 8/10
- Pain radiates to anterior leg, aggravated by movement
- Clinically vital signs stable, no fever, no neurological deficit of both lower limbs
- Tenderness at right paravertebral region with mild bulge, no spine tenderness, no wound, no gibbus
- Limited right hip and knee movement and range of motion due to pain
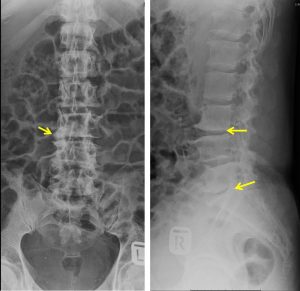
X-Ray findings:
- Loss of normal lumbar lordosis
- Vertebral body heights are normal
- There is reduction in L3/L4 and L5/S1 disc spaces, more prominent on the right side
- Vertebral end plates sclerosis and irregularity are also seen at this levels
- Multilevel osteophytes formation are seen. Pedicles are intact
- No obvious soft tissue swelling
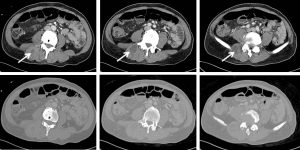
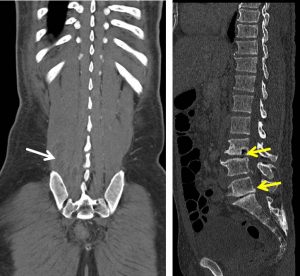
CT scan findings:
- Multiloculated rim enhancing collections is present at right paraspinal muscles from L3 inferior end plate level until the S1 level (white arrows).
- The largest collection appears to be originating from the adjacent L3/L4 intervertebral space. The L3/L4 intervertebral space particularly on the right side is reduced (yellow arrows). Sclerosis of the inferior end plate of L3 and superior end plate L4 is also observed. Similar finding (reduced intervertebral space and end plate sclerosis) is also seen at L5/S1 level.
- The involved vertebral body height is still preserved. However there is evidence of L4 right lamina erosion.
- The left psoas muscle is normal.
- No abdominal/pelvic lymphadenopathy.

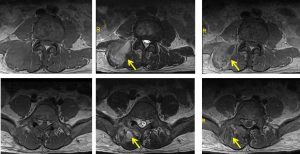
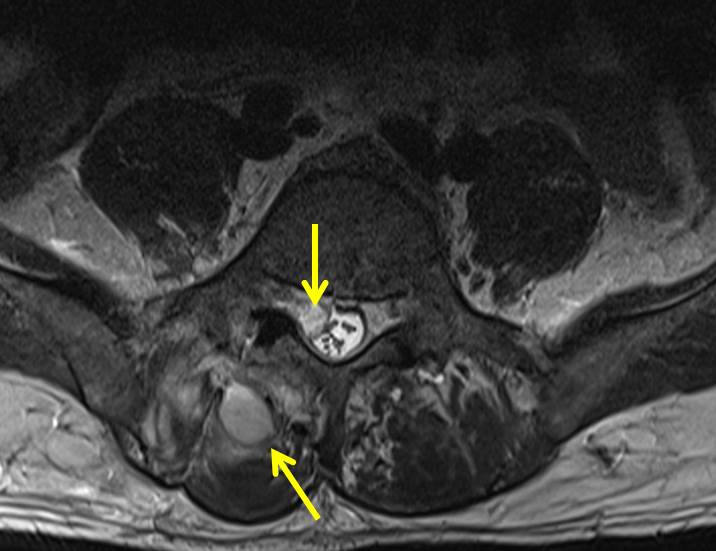
MRI findings:
- Cortical destruction is noted at inferior L3 and superior L4 end-plates. Ill-defined lesion is seen within L3 vertebra adjacent to the inferior end-plate. Another smaller lesion is also noted at inferior end-plate of L5. These lesions are heterogeneously hypointense on T1W, T2W and TIRM with heterogenous enhancement post contrast.
- Heterogenous high T2W/ TIRM marrow signal intensity suggestive of marrow oedema is observed involving L3, L4, L5 and S1 vertebral body.
- The rest of vertebrae return normal marrow signal intensity with no focal lesion within.
- Ill-defined multiloculated collections are observed within the right erector spinae muscle group. The largest collection is observed extending from L3/4 level until L5 level.
- Another smaller collection is noted at right sacrospinalis muscle.
- Extension of this collection is observed into the epidural space of vertebral canal through the right neural foramen at L5/S1 level, thus, indenting the theca sac and causing narrowing of spinal canal at this level. This intraspinal collection extends inferiorly until S1/S2 level, causing impingement of right S1 exiting and S2 traversing nerve roots.
- No intra-abdominal or intra-peritoneal extension of collection is seen.
- No collection is seen within right quadratus lumborum and psoas muscles.
Progress of patient:
- Percutanous CT drainage of the abscess was done.
- Pus aspirated-culture and sensitivity shows Staph. Aureus, sensitive to cloxacillin
- Completed 14 days of IV cloxacillin
- TB screening and investigations are negative
- Repeat CT scan after 5 weeks shows resolution of abscess
Diagnosis: Pyogenic spondylodiscitis with right paraspinal abscess.
Discussion:
- Pyogenic spondylodiscitis is infection that includes osteomyelitis, spondylodiscitis and epidural abscess.
- Commonly occur in male in their fifth decades
- Risk factors include sepsis, DM, immunosuppression and substance abuse
- Most common causative organism is Staphylococcus aureus and Streptococcus spp.
- Can occur anywhere but commonly at lumbar spine
- Single level involvement occur in 65% of cases, multiple contiguous levels in 20% and multiple non-contiguous levels 10%.
- Plain radiograph may shows disc spaces narrowing and irregularity of vertebral end plates.
- CT findings are similar to radiograph but more sensitive to see changes of surrounding soft tissues such as paraspinal and psoas muscle abscesses.
- MRI is more sensitive to demonstrate marrow oedema, epidural collection and surrounding soft tissue involvement or extension.