Case contribution: Dr Radhiana Hassan
Clinical:
- A 53 years old man, with underlying nasoparyhngeal carcinoma diagnosed and completed chemotherapy and radiotherapy 7 years ago.
- HPE shows moderately differentiated keratinizing squamous cell carcinoma (WHO type 1).
- He recently presented with headache, vomiting, fever, and altered mental status (E4V4M5). He started to have fitting episodes since last year.
- Patient currently complains of frequent seizures, but symptoms controlled after the increment dosage of anti-epileptic (on T. Keppra 1.5g BD and C. Phenytoin 300mg ON)
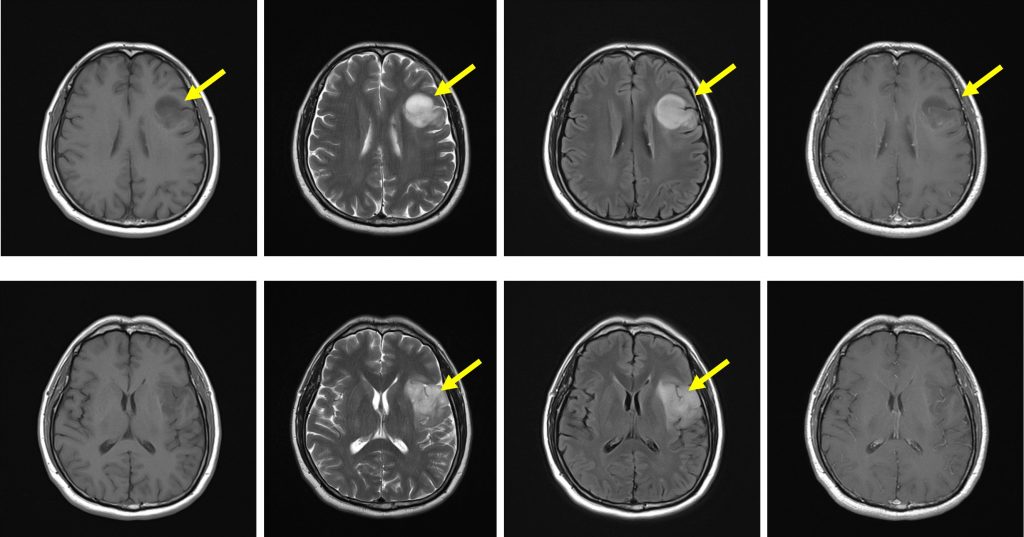
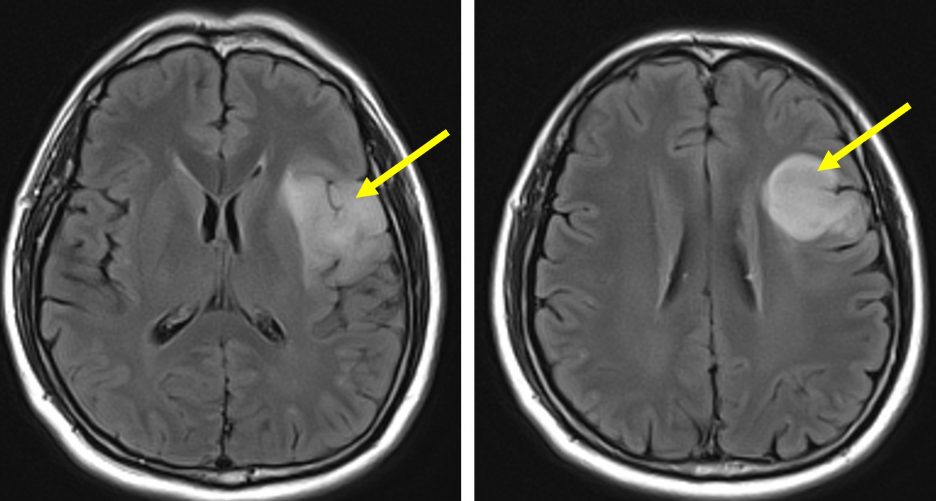
MRI findings:
- There is an area with abnormal signal intensity at left fronto-temporal lobe
- It has well-defined margin and hyperintense on T2/FLAIR sequence
- It is hypointense on T1-weighted image with no enhancement post gadolinium
- No significant mass effect. No midline shift.
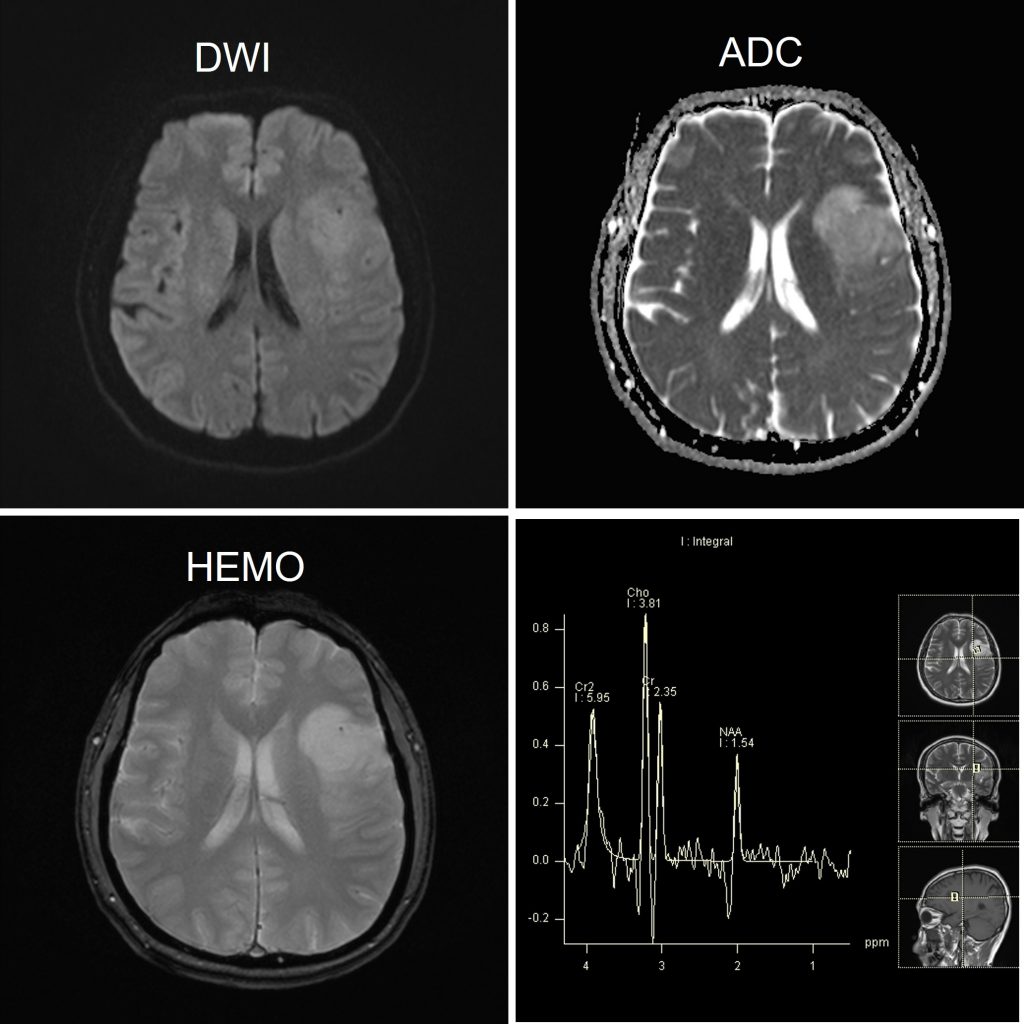
- No blooming artefact or restricted diffusion
- Reversel of Cho-NAA peak on MR spectroscopy
- No lactate or lipid peak
Diagnosis: Low grade glioma (astrocytoma)-presumed diagnosis
Discussion:
- The development of neoplasms subsequent to therapeutic cranial irradiation is a rare but serious and potentially fatal complication.
- All tumours arose within the previous radiation fields and related to radiation dose received.
- Thus, in nasopharyngeal carcinoma temporal lobe is the most likely site of tumour occurence.
- The median latency period before the detection of the secondary tumour was 14.5 years (range: 6.5-24 years).
- One study showed that meningiomas is the commonest type followed by sarcomas and malignant gliomas.
- In this case there is no definite evidence that the glioma is secondary to previous irradiation as no detail information about previous radiotherapy is available