Case contribution: Dr Radhiana Hassan
Clinical:
- A 29 years old Malay lady, no known medical illness
- Presented with progressive blurred vision associated with headache, retro orbital pain and vomiting
- Clinical examination shows bitemporal inferior quadrantopia
- Patient also has hypothyroidism and hypocortisolism
- Proceed with endoscopic transphenoidal hypophysectomy.
- However, unable to fully excise tumor in view of close proximity to ICA.
- Post operatively visual field improving. Previous bitemporal hemianopia resolved.
- Patient was discharged well with hormonal replacement therapy (hypocortisolism, hypogonadotrophic hypogonadism, hypothyroidism).
- Patient presented with headache and blurred vision after 3 months post operation.
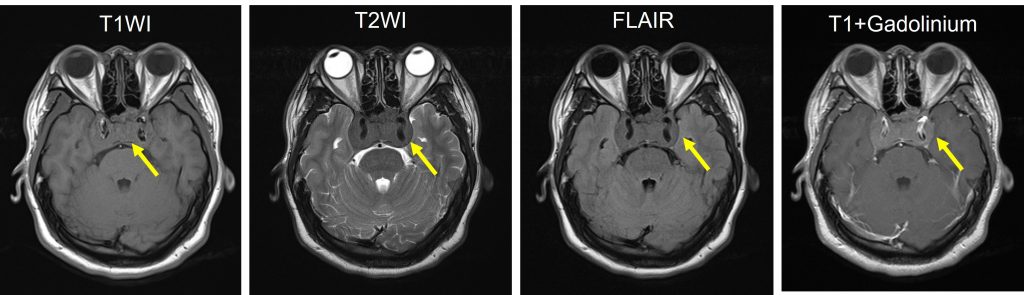
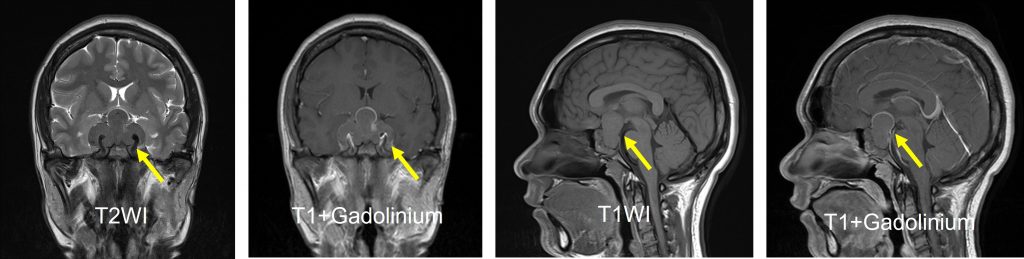
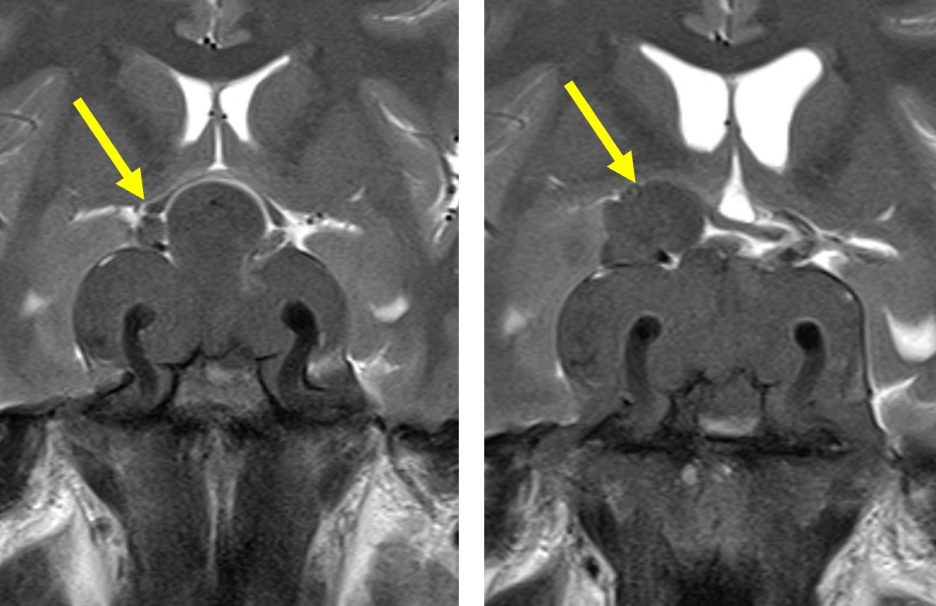
MRI findings:
- A large sellar mass extending to suprasellar region
- It is isointense on T1WI, hypointense on T2WI and shows homogenous enhancement post contrast
- Invasion to cavernous sinus with encasement of both ICAs
- Both ICAs are patent
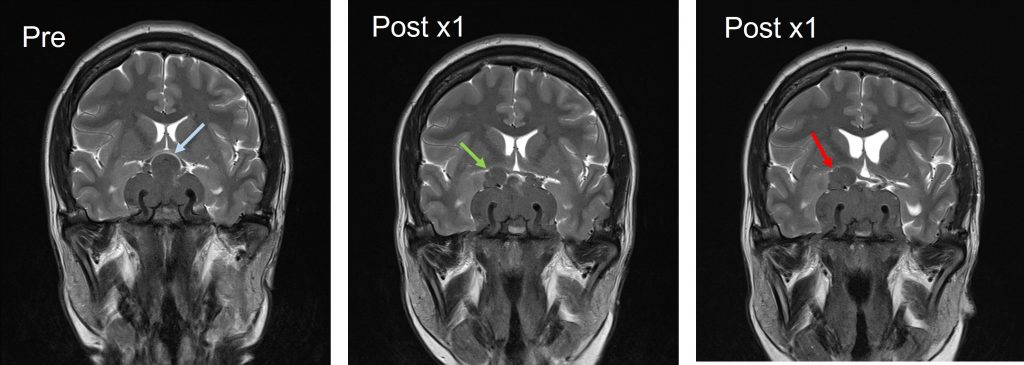
Diagnosis: Residual and recurrent non-functioning pituitary adenoma (HPE-proven)
Discussion:
- Non-functioning pituitary adenoma (NFPA) is the most frequent type of pituitary tumour
- It often presents as a macroadenoma larger than 10mm
- It can cause symptoms related to mass effect i.e compression of the optic apparatus causing bitemporal hemianopia.
- Patients can have hypopituitarism secondary to compression of the normal pituitary gland.
- Transphenoidal surgery is the treatment of choice.
- Recurrence of NFPA occurs between 1-5 years after surgery and decreases after 10 years.
- Suprasellar extension is commonest, followed by cavernous sinus and infrasellar in
- Residual or recurrent tumour can be treated with radiotherapy, stereotactic radiosurgery or repeat surgery.