Case contribution: Dr Radhiana Hassan
Clinical:
- A 22 years old man
- No known medical illness, presented with bilateral lower limb weakness, LL>UL
- Associated with blurring of vision
- The symptoms progressively worsen over one week
- Clinically muscle power of both upper and lower limbs were 2/5
- Reflexes normal, treated as demyelinating disease, with IVIG and methylprednisolone
- Referred to other hospital for expert opinion since his condition not improved
- Subsequently diagnosed as GFAP demyelination disease (pending investigation result)
- Patient shows good response to IV rituzimab, latest clinical examination shows muscle power of 4/5
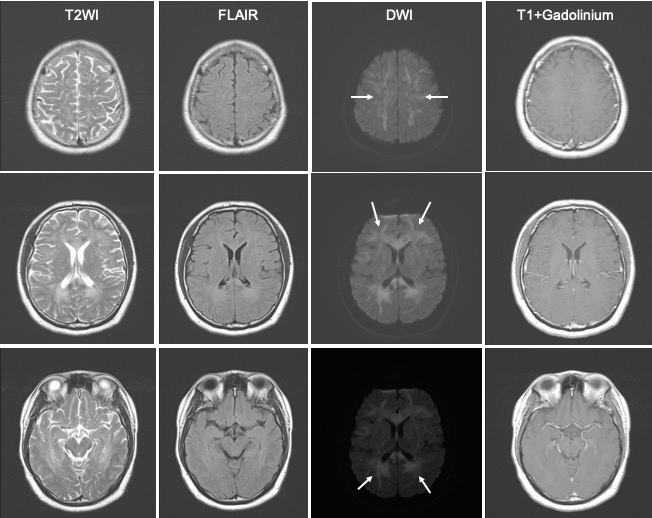
MRI findings:
- Abnormal T2/FLAIR hyperintensity is seen in the white matter
- Bilateral, almost symmetrical involvement, some confluent areas
- Involvement of periventricular white matter, centrum semiovale, corpus callosum
- The lesions show restricted diffusion, no enhancement
- MRI spine done was normal (image not shown)
- Optic nerves are also normal (images not show)
- The changes show more extensive involvement on subsequent imaging, otherwise signal intensity remain the same
- No enhancement and no change in restricted diffusion areas
Diagnosis: GFAP astrocytopathy (presumed diagnosis, awaiting final lab results)
Discussion:
- GFAP astrocytopathy is a rare inflammatory CNS disorder
- It tends to occur in middle-aged adults with slight female preponderance
- It has broad neuropsychiatric and temporal spectrum clinical presentation
- The pathophysiology is not well understood.
- The key marker is GFAP antibody which has a higher positive predictive value when present in CSF rather than in the serum.
- Co-existing NMDA receptor antibody, aquaphorin-4 antibody may also be present
- MRI features include T2/FLAIR hyperintensity which is diffuse, confluent at periventricular white matter often extending to centrum semiovale, deeper brain structures and or brainstem.
- It may also shows perivascular enhancement extending radially from the periventricular surface. Less characteristic is leptomeningeal or periependymal enhancement.
- Optic nerve often normal on imaging.
- MR angioram is also normal. No restricted diffusion on DWI and ADC.
- Findings can also involve spinal cord.
- A differential diagnosis for this case was acute demyelination lesions with restricted diffusion in MS; a new variant of MS lesion. However, the lesions do not show resolving restricted diffusion after treatment.