Case contribution: Dr Radhiana Hassan
Clinical:
- A 12 years old girl with underlying ASD (atrial septal defect)
- Presented with fever and altered behaviour one week after COVID-19 vaccination
- CT scan brain done revealed cerebral oedema with impending internal herniation
- Urgent craniotomy and EVD insertion was done
- She was referred for further management from other hospital
- MRI brain was performed
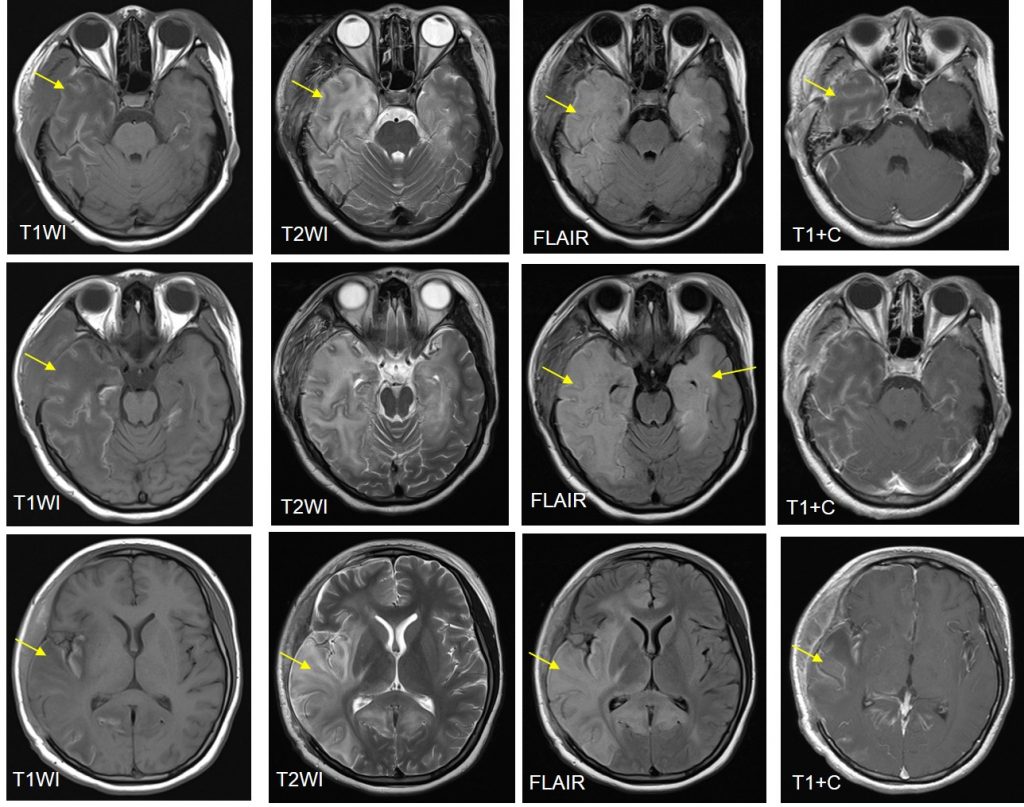
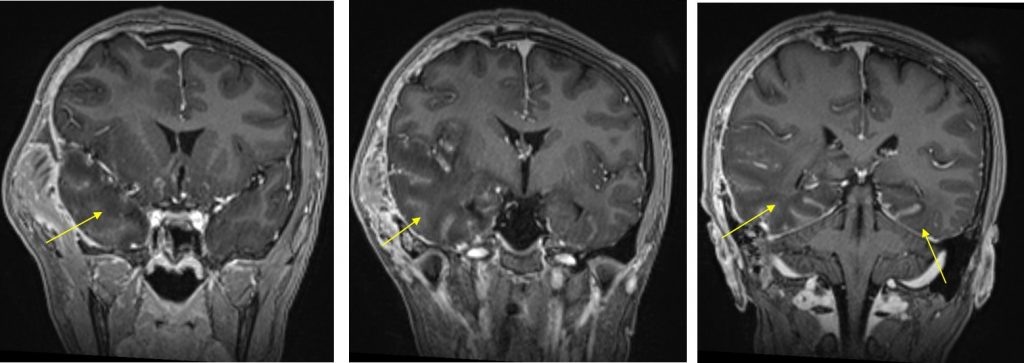
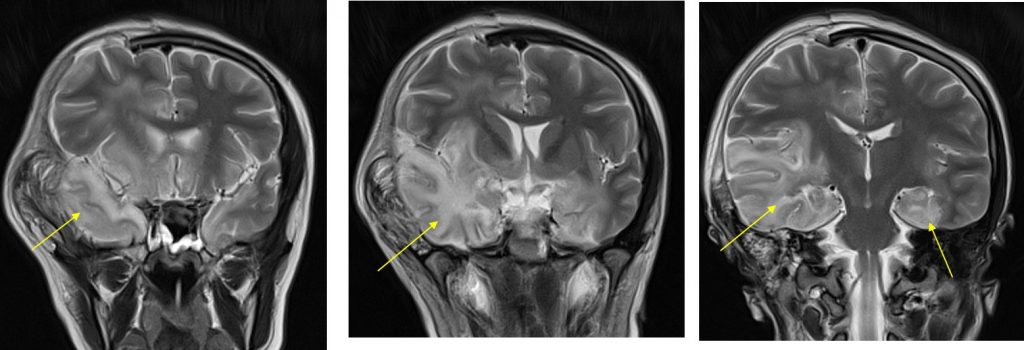
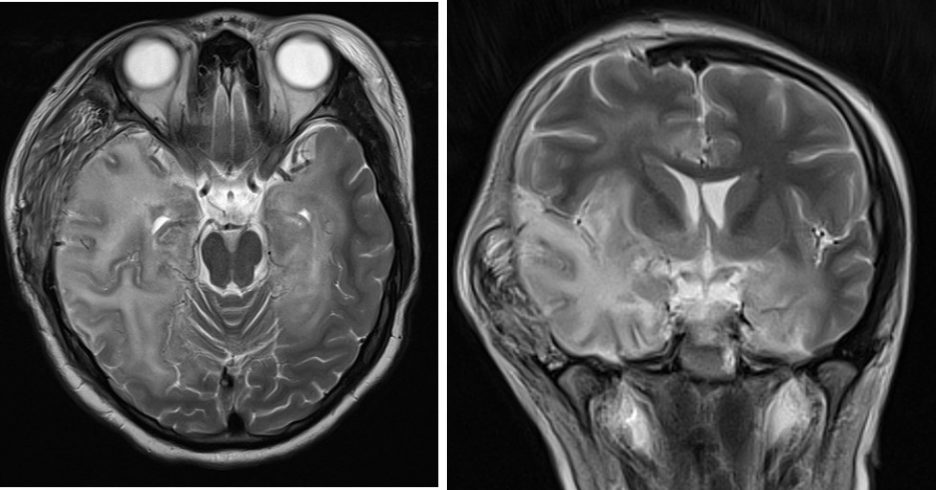
MRI findings:
- Extensive abnormal signal intensity is seen in the temporal lobes, inferolateral frontal lobes and insula cortex
- Involvement is bilateral but asymmetrical, worse on the right side
- It is hypointense on T1, hyperintense on T2 and FLAIR with minimal contrast enhancement post contrast
- Sparing of basal ganglia is seen
- Craniectomy defect and post operative changes are also seen
- No hydrocephalus on current images (previous CT scan images were not available)
Diagnosis: Herpes simplex encephalitis
Progress of patient:
- Patient responded well with treatment
Discussion:
- Herpes simplex encephalitis is the most common cause of fatal sporadic necrotizing viral encephalitis
- In adolescent/adult type, it is commonly caused by Type 1 herpes simplex virus (>95% of cases).
- MRI shows abnormality involving the cortical and subcortical regions of bilateral temporal, frontal lobes and insula region. Involvement of extratemporal regions, cingulate gyrus can also be seen.
- Involvement is bilateral and asymmetrical
- Basal ganglia is usually spared, an important feature to differentiate with MCA infarction.
- There may be associated with restricted diffusion, gyral swelling, loss of gray-white matter interface with mild or no enhancement.