Case contribution: Dr Radhiana Hassan
Clinical:
- A 29 years old lady
- Underlying myasthenia gravis on treatment
- Current presentation of proximal myopathy for one month
- To look for thymoma
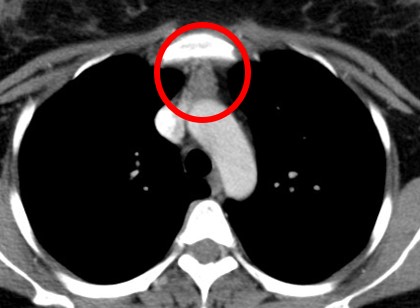
CT scan findings:
- A soft tissue structure (mean HU 54) is located in between the sternum and mediastinal great vessels.
- It has well-demarcated margin and triangular in configuration with homogenous mild enhancement.
- No associated cystic component or intralesional calcification.
- It maximal thickness measures 1.5 cm (normal thickness is equal or less than 1.3 cm in adult patient).
HPE findings:
- Macroscopy: well-encapsulated tissue partly covered by fatty tissue. On cut section shows yellowish cut section with multiple areas of hemorrhage largest measuring 15 mm and cystic spaces measuring 5 mm.
- Microscopy: section shows hemorrhagic thymic tissue composed of mild expansion of medulla and disordered epithelial cells with Hassel corpuscle. The medulla is surrounded by cortex consist of lymphoid cells with tangible body macrophages. The hemorrhage is seen in both the cortex and medulla. Fatty tissue is observed in between thymic lobules. Areas of calcification are noted. No atypical cells or malignancy seen.
- Interpretation: Hemorrhagic thymus hyperplasia
Discussion:
- In frontal chest radiograph of infant and young children, the thymus is strikingly large but difficult to discriminate from the cardiac sillhoutte. It usually forms a smooth border and remains visible through the age of 3 years.
- The thymic wave sign which is a scalloped or wavy contour of the organ is created by impression of the ribs.
- The thymic sail sign is caused by impression of the minor fissure causing a triangular slightly convex right lobe of the thymus with sharply demarcated base.
- On ultrasound, normal thymus in infarnts may have multiple linear or branching echogenic foci with homogenous echogenicity similar to liver and spleen in majority of cases. In older children, the echo pattern appears as a fine mixture of remaining lymphoid tissue and fat. It is very pliable and does not compress or displaced the adjacent structures.
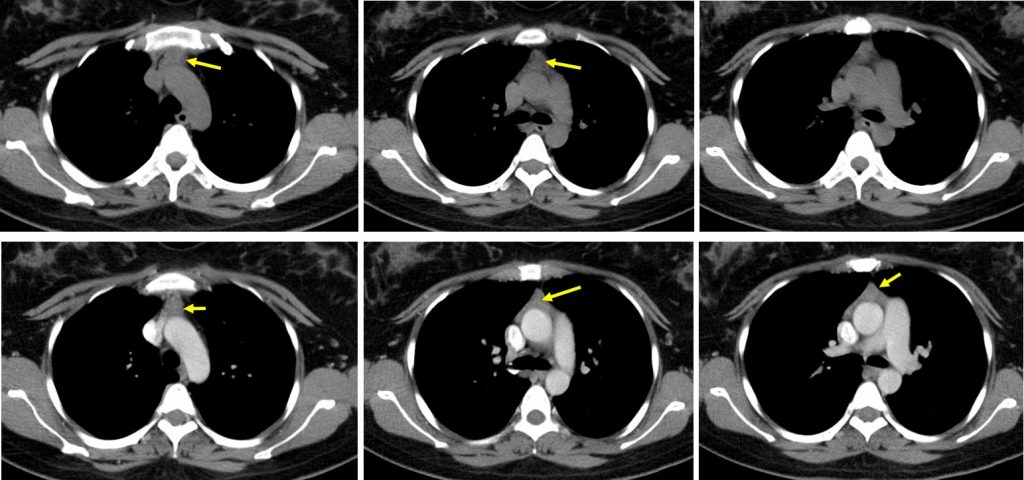
- ON CT scan, thymus is visible at the perivascular space throughout the first two decades of life. In children younger than 5 years, the thymus appears quadrilateral with convex borders. As the child grows, the thymus gradually becomes triangular with straight or concave borders.
- At MRI the thymus appears homogenous with signal intensity greater than muscle on T1WI and signal intensity close to fat on T2WI.
- Thymic hyperplasia is characterized by an increase in size and weight of the thymus with normal preservation of its organized microscopic feature. It usually retain its normal shape or may appear oval in shaped instead of its distinct bilobed appearance.
- True thymic hyperplasia can occur in those without related pre-existing condition and those with other conditions such as SLE, sarcoidosis or hyperthyroidism.
- Thymic lymphoid hyperplasia is characterized by the presence of hyperplastic lymphoid germinal centre in the thymic medulla that is associated with lymphocytic and plasma cell infiltration. Unlike true hyperplasia, lymphoid hyperplasia may occur with or without thymic enlargement. It is commonly associated with autoimmune disease such as myasthenia gravis, thyrotoxicosis and connective tissue disease.
- However these two conditions is difficult to be distinguished based on imaging findings alone. Certain studies show that lymphoid thymic hyperplasia have higher HU values (>40) compared to true thymic hyperplasia.
- Imaging features suggestive of hyperplasia rather than normal thymus include
- Presence of convex border after 19 years of age
- Presence of soft tissue lobulation
- Presence of soft tissue masses
- Increased thickness, should not be >1.3cm beyond 20 years old