Case contribution: Dr Radhiana Binti Hassan
Clinical:
- A 57-years old lady, newly diagnosed DM presented with reduced effort tolerance for 6 months.
- Clinical examination showed diffuse goitre. No thyrotoxicosis symptoms.
- Anterior neck swelling for 3 years with ho hyperthyroid symptoms and no aerodigestive symptom.
- Had undesired weight loss of 10 kg within 1 year
- No altered bowel habit
- Blood investigation: anemia. Others are normal.
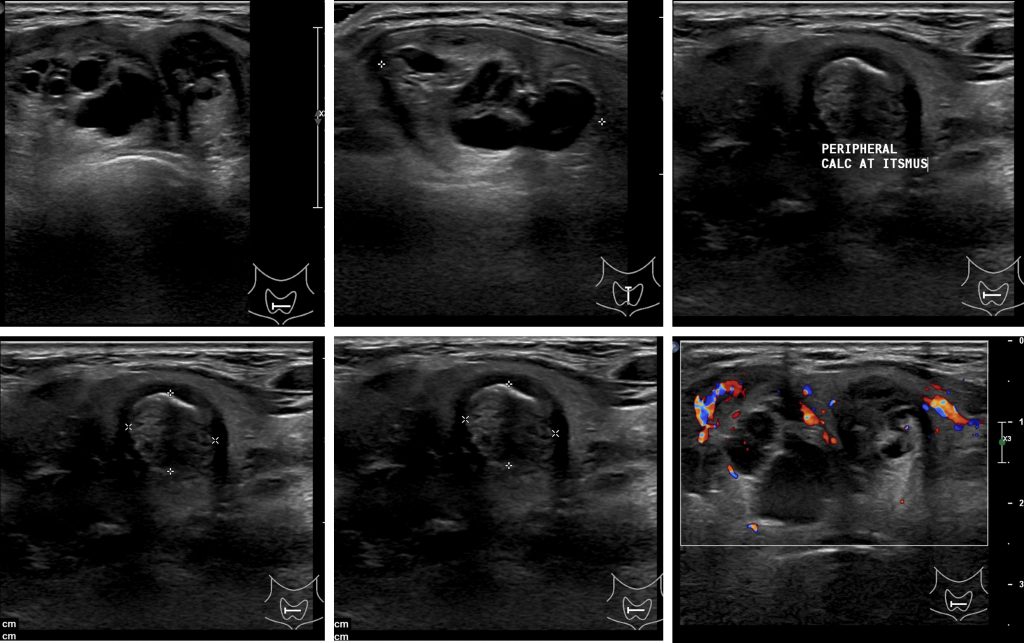
Ultrasound findings:
- The thyroid gland is enlarged. The parenchyma is heterogenous.
- There are multiple well defined thyroid nodules of mixed and solid cystic in composition of varying sizes seen in right and left thyroid lobe.
- No intralesional calcification noted within.
- No significant intralesional vascularity is detected.
- No retrosternal extension.
- There are bilateral subcentimeter cervical lymph nodes with preserved fatty hilum seen measures up to 0.7 cm in short axis (left cervical).
- Both IJV and CCA are seen patent.
FNAC of thyroid nodules performed:
- Result: Benign follicular nodule with cystic degeneration
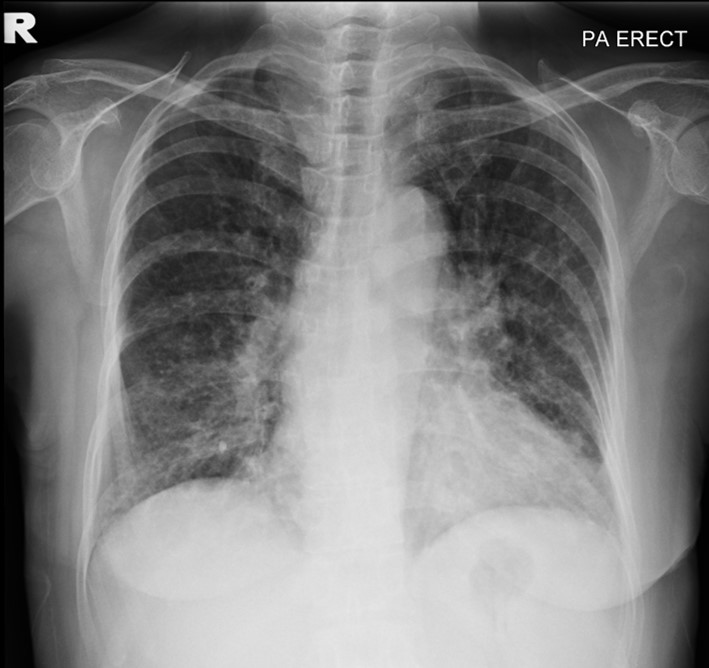
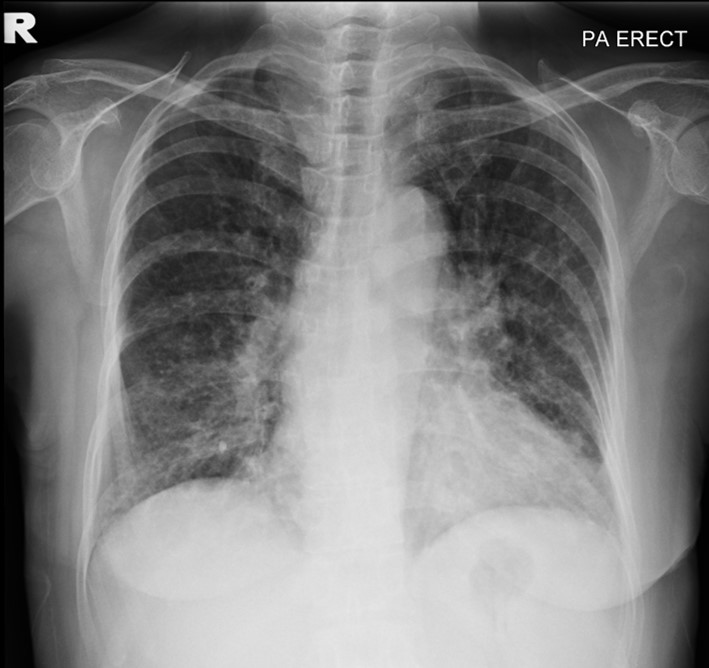
Chest radiograph findings:
- Generalised reticulonodular lesions, mainly at both lower zones.
- No consolidation. No cavitating lung lesion.
- No pleural effusion. No pneumothorax.
- Lobulated hilum on the left side.
- Mediastinum is normal.
- Cardiomegaly with cardiothoracic ratio of 0.6.
- The visualized bones and soft tissues are unremarkable.
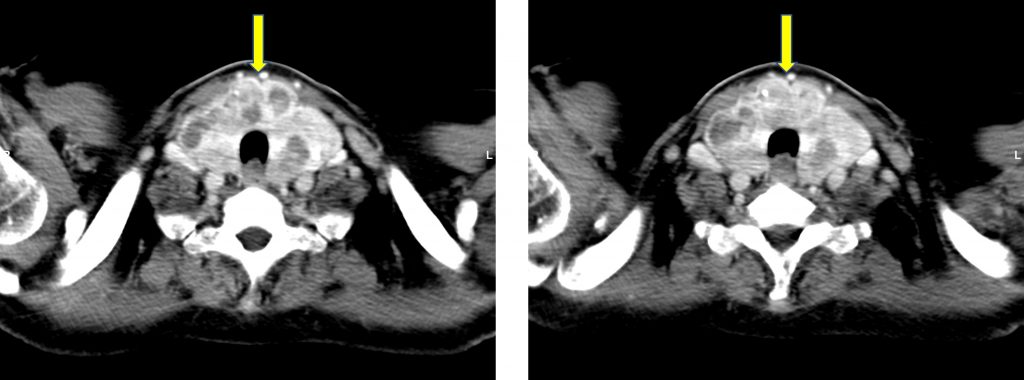
CT scan findings:
- CT scan was performed to assess for lymphadenopathy as blood film showed presence of lymphoplasmacytic cells.
- Pre- and post IV contrast CT neck, thorax, abdomen and pelvis were acquired.
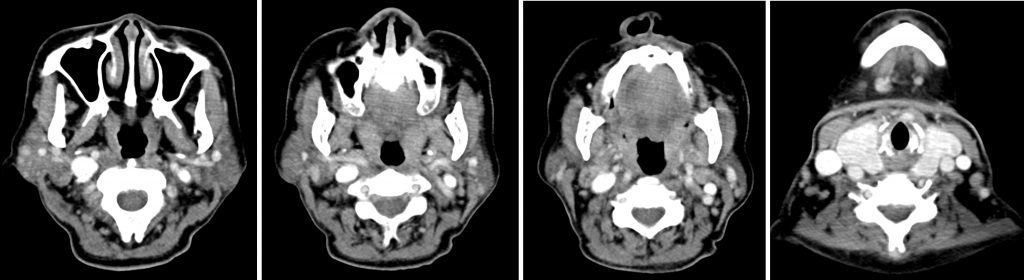
- The thyroid gland is enlarged with multiple well defined hypodense lesions seen within (yellow arrow)
- Several enlarged cervical lymph nodes at bilateral level Ia, Ib, II, III and level IV with the largest at the right level II measuring 1.4 cm in short axis diameter (SAD). Some of the enlarged nodes show matted appearance.
- Subcentimeter lymph nodes are also seen in bilateral parotid glands.
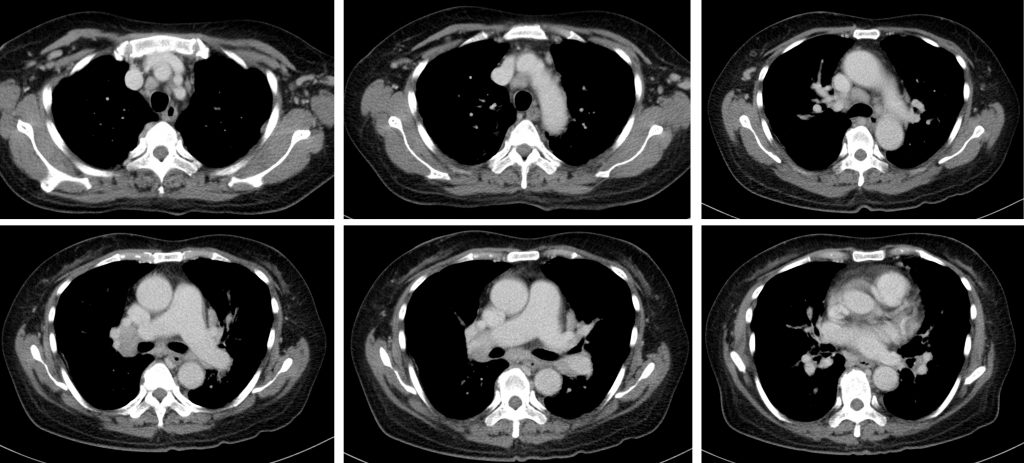
- Multiple enlarged mediastinal lymph nodes with the largest at the 4R station measuring 1.6 cm in short axis diameter. Presence of enlarged matted lymph nodes are also noted at the right hilar region.
- Several enlarged axillary lymph nodes
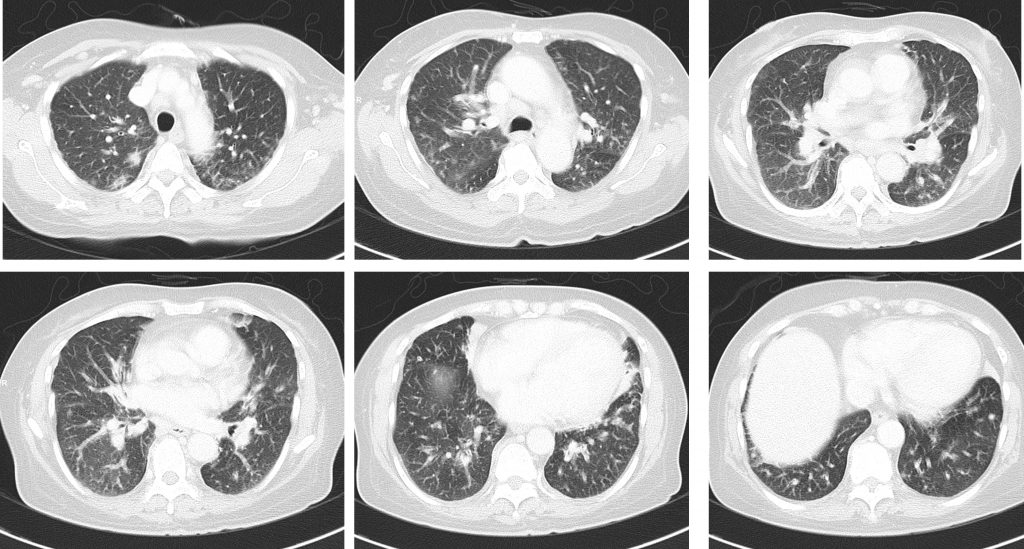
- Multiple tiny lung nodules with patchy ground glass opacities scattered in both lungs, mainly peripheral location.
- There are septal thickenings. No pleural effusion
- Multiple enlarged lymph nodes are observed at the paraaortic region
- Enlarged pelvic lymph nodes are also noted with the largest at the left external iliac region.
Biopsy of right inguinal nodes:
- sections show lymphoid follicles with atretic and slightly hyalinized germinal centers. The mantle zone shows onion skinning and prominent penetrating venules forming ‘lollipop’ follicles. There is marked expansion of the interfollicular area by sheets of mature plasma cells. No plasmablastic cells or Russle bodies seen. No atypical cells are seen.
- Immunohistochemistry: The lymphoid follicles are small and highlighted by CD20 with preserved FDC meshwork as highlighted by CD21. The Ki67 and CD10 highlights the immunoarchitecture of regressed germinal centres. Reactive T cells within the interfollicular are highlighted by CD3 and CD5. The sheets of plasma cells are positive for CD138 and negative for CD20 and CD56. No kappa or lambda light chain restriction.
- Interpretation: Consistent with Castleman disease, plasma cell variant.
Final Diagnosis: Multicentric Castleman Disease
Treatment:
- IV RItuzimab
- EP 4000 unit
- T. COrticosteroid
Discussion:
- Castleman disease is also known as angiofollicular lymph node hyperplasia or giant lymph node hyperplasia
- It is an uncommon benign B-cell lymphoproliferative condition.
- Unicentric Castleman disease typically occurs in children and young adults (3rdand 4th decades), with a slight female predominance (1.4:1) 15.
- Multicentric Castleman disease, on the other hand, occurs in an older population (5th and 6th decades), with a slight male predominance 15. HIV is a relevant risk factor for this condition, and it has been demonstrated that all the HIV patients with multicentric Castleman disease are coinfected with the human herpesvirus 8 (HHV-8).
- Associations: POEMS syndrome, osteosclerotic myeloma, Kaposi sarcoma, AIDS, amyloidosis, chordoid meningioma.
- Multicentric Castleman disease has an exuberant clinical presentation due to the systemic inflammation, with symptoms such as fevers, night sweats, fatigue, and weight loss, and clinical signs of generalized lymphadenopathy, hepatosplenomegaly, and fluid retention.
- Hematological abnormalities such as anemia, elevated inflammatory markers, hypergammaglobulinemia, and hypoalbuminemia are commonly found in patients with multicentric Castleman disease.
- Plain radiograph: Thoracic lesions may present as mediastinal masses. Additional findings include the following: displacement of adjacent structures due to mass effect, ipsilateral pleural effusion, periosteal reaction.
- Ultrasound: findings are non-specific, mostly hypoechoic mass or nodules and indistinguishable from other causes of lymphadenopathy.
- Typical thoracic Castleman’s disease usually occurs in the mediastinum and hilum and manifests as a rounded solitary mediastinal or hilar mass in asymptomatic patients. On chest radiographs, mediastinal Castleman’s disease may mimic thymoma, lymphoma, or neurogenic tumor. Uncommonly, thoracic Castleman’s disease arises from other locations, including the pleura, pericardium, intercostal space, and lung, with atypical imaging features. Pleural Castleman’s disease may present as either a well-defined interlobar mass or massive pleural effusion.
- Intrapulmonary Castleman’s disease may appear as a solitary lung mass.
- Most instances of abdominal or pelvic Castleman’s disease may not be visible on abdominal radiographs unless they are massive or calcified.
- Conversely, multicentric Castleman’s disease may manifest as bilateral hilar and mediastinal enlargement , diffuse reticulonodular pulmonary infiltrations, hepatosplenomegaly, and ascites.