Clinical:
- A 9-year-old girl who was previously diagnosed with Langerhans cell histiocytosis.
- Previous assessment showed bony and pulmonary involvement.
- Recently she also developed diabetes insipidus.
 MRI findings:
MRI findings:
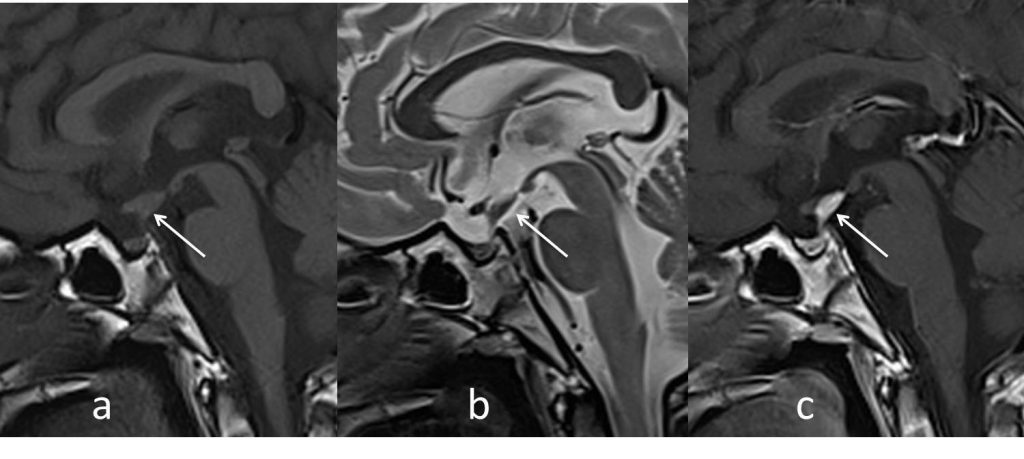
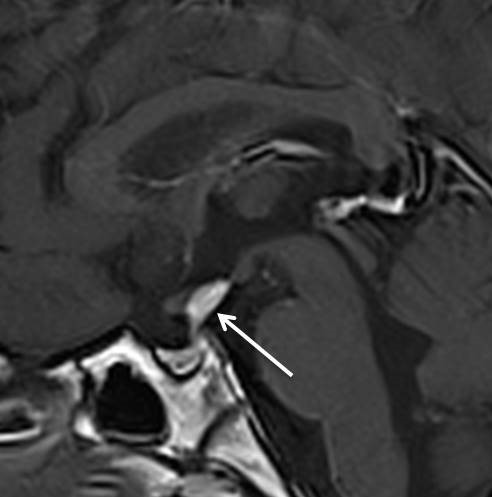
- The MRI in sagittal (a) T1-weighted, (b) T2-weighted and (c) T1 post gadolinium images
- Abnormal thickening of the pituitary stalk (white arrow).
- The thickened pituitary stalk shows homogenous vivid enhancement post contrast.
- There is absent of normal posterior pituitary bright spot on T1W-images.
- Pituitary gland is normal in size.
Diagnosis: Pituitary stalk Langerhans cell histiocytosis
Discussion:
- Langerhans cell histiocystis (LCH) is a rare disease with multisystem/multiorgan involvement.
- The incidence is more common in children. Estimated incidence of 5 per million children and 1-2 cases per million adult population.
- The most common CNS manifestation in LCH is infiltration of the hypothalamic-pituitary region by LCH granuloma. This frequently results in diabetes insipidus.
- Diabetes insipidus may occur before, simultaneously and after the other multisystem manifestations, making the diagnosis difficult.
- Since the etiological diagnosis of central DI with thickening of the pituitary stalk may not be apparent at the time of detection of DI, serial imaging and close follow-up of these patients to reach a conclusive diagnosis is necessary and mandatory to avoid the attendant risks of pituitary stalk biopsy
- Radiological manifestations of the disease include thickening of pituitary stalk more than 3 mm, with loss of physiological hyperintense signal in posterior pituitary on T1W images signifying loss of ADH storage granules. This may progress to a mass lesion involving pituitary and hypothalamus.
- Other less common CNS manifestations are neurodegenerative changes and intra axial mass lesions.
Recent Comments