Case contribution: Dr Radhiana Hassan
Clinical:
- A 64 years old male
- Underlying hypertension for 10 years on medication
- History of right CVA 2 years ago with no residual weakness, on aspirin
- On investigation for gastritis
- Noted abnormal CXR
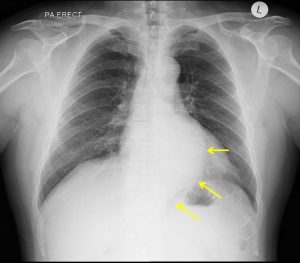
Radiograph findings:
- A well-defined opacity is seen at retrocardiac region (yellow arrows)
- in continuation with descending aorta outline
- No abnormal wall calcification is seen.
- No blunting of costophrenic angle
- No other significant finding
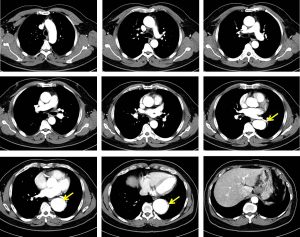
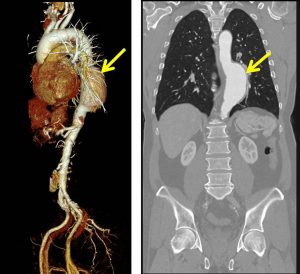
CT angiography findings:
- There is a fusiform aneurysmal dilatation of the descending thoracic aorta
- The maximal AP diameter measures about 4.9 cm and the length is 8.8 cm.
- No feature to suggest of impending rupture.
- No intimal flap is demonstrated to suggest dissection.
- The aneurysm commenced about 9.9 cm beyond the origin of left subclavian artery. The left subclavian artery itself appears normal, with no aneurysmal dilatation or dissection. The brachiocephalic and right subclavian branches of the arch of aorta are also normal.
Diagnosis: Descending thoracic aorta aneurysm (Standford B)
Discussion:
- Thoracic aneurysms may involve one or more aortic segments (aortic root, ascending aorta, arch, or descending aorta) and are classified accordingly.
- Sixty percent of thoracic aortic aneurysms involve the aortic root and/or ascending aorta, 40% involve the descending aorta, 10% involve the arch, and 10% involve the thoracoabdominal aorta (with some involving >1 segment).
- Most patients with thoracic aortic aneurysms are asymptomatic at the time of diagnosis, because the aneurysms are typically discovered incidentally on imaging studies
- Diagnosing requires a CT scan and regular CT scans every 6 months or one year to monitor for growth.
- In general, the term aneurysm is used when the axial diameter is >5.0 cm for the ascending aorta and >4.0 cm for the descending aorta.
- There is about 10% prevalence of association with intracranial aneurysm
- Treatment may include minimally invasive surgical techniques such as stenting.
Progress of patient:
- Confirmed gastric adenocarcinoma with mass lesion at lesser curvature until prepyloric region
- Underwent staging laparoscopy, laparotomy and gastrojejunostomy bypass with uneventful recovery
- Currently on chemotherapy
- Aneurysm under surveillance by vascular team

Recent Comments