Case contribution: Dr Radhiana Hassan
Clinical:
- A 72 years old man
- Underlying DM and hypertension on medication
- Presented with generalised weakness and drooling of saliva
- No fever or loss of appetite, loss of weight, no trauma
- Went to a private hospital, urgent CT brain shows a mass lesion in the brain
- Referred for further management in our centre
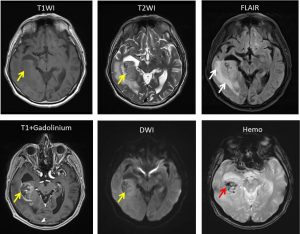
MRI findings:
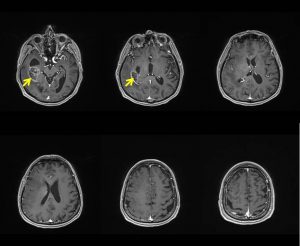
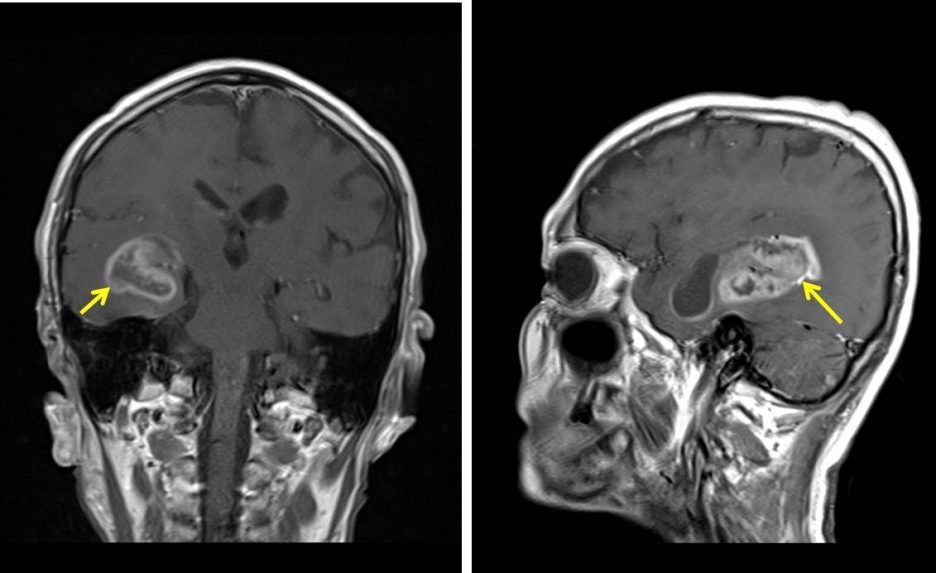
- There is a heterogeneous, lobulated supratentorial intra-axial mass seen arising from the white matter of the right temporal lobe (yellow arrows).
- The mass measures approximately 4.1 x 3.1 x 2.5 cm (AP x W x CC).
- The mass appears heterogeneously hypointense on T1, heterogeneously hyperintense on T2 and FLAIR with no areas of restricted diffusion on DWI/ ADC.
- Post IV Gadolinium, the mass demonstrates peripheral ring enhancement with areas of central necrosis.
- Presence of perilesional vasogenic oedema is also seen (white arrows).
- Multiple foci of hypointense signals are seen within the mass with corresponding blooming artifacts indicative of hemosiderin deposition (red arrows).
- Laterally, the mass appears to compress the adjacent temporal lobe parenchyma with sulcal effacement.
- Medially, the mass compresses the ipsilateral lateral ventricle causing compensatory dilatation of the right temporal horn of the lateral ventricle as well as right uncal herniation.
- No midline shift.
Progress of patient:
- Right burr hole and biopsy done
- Greyish tissue biopsied
- Discharged home 2 days later and referred to other centre for further treatment
HPE findings:
- Macroscopy: specimen labelled as brain tumour consist of whitish and brownish tissues
- Microscopy: section shows multiple fragments of tumour tissue with large area of necrosis. The tumour is hypercellular and is composed of neoplastic cells displaying pleomorphic nuclei, vesicular to hyperchromatic nuclei, occasional prominent nucleoli, and scanty to moderate amount of cytoplasm. Mitosis is present with mitotic count of 3 mitoses/10hpf. Microvascular proliferation is prominent with glomeruloid appearance. Scattered gemistocytes are seen.
- Immunohistochemistry: the cells are positive for GFAP. The proliferative index (Ki-67) is 10-20%.
- Interpretation: Glioblastoma (WHO Grade IV)
Diagnosis: Glioblastoma multiforme
Discussion:
- Glioblastoma multiforme is the most common primary malignant tumour in adults.
- It may arisi de novo or may develop through malignant transformation of low grade astrocytoma.
- The peak incidence is at 65 years old but it is found in any age groups with slight male predominance.
- Most commonly located in the deep supratentorial white matter, it is uncommon in posterior fossa and spinal cord.
- It is seen on MR as heterogenous lesion with–innermost region=central hypoT1 and hyperT1
–Solid region- viable, fleshy and hypercellular with abundance neovascularity= contrast enhancement forming an irregular ring with thick walls of varying width and shaggy inner margin
- MRI features that distinguish the anaplastic Grade 3 astrocytoma from glioblastoma grade 4 is hemosiderin deposits or other evidence of prior hemorrhage.
- Perilesional vasogenic oedema is commonly seen.
Recent Comments