Case contribution: Dr Radhiana Hassan
Clinical:
- A 58 years old female with underlying diabetes and hypertension
- Presented with lethargy, headache, vomiting for the past 1 week.
- Headache was throbbing in nature with pain score 3/10 and is associated with neck stiffness and photophobia.
- No limb weakness no fever. No constitutional symptoms.
- Clinical examination shows GCS E4V5M6. Pupils 3/3 reactive
- CVS/lung/abdomen examination normal.
- Breast examination – no mass palpable
- Power left upper and lower limb 4/5
- Cerebellar sign positive. Dysdiadochokinesia positive over right side
- No pass pointing. No intention tremors
- FBC/RP/Coagulation profile normal.
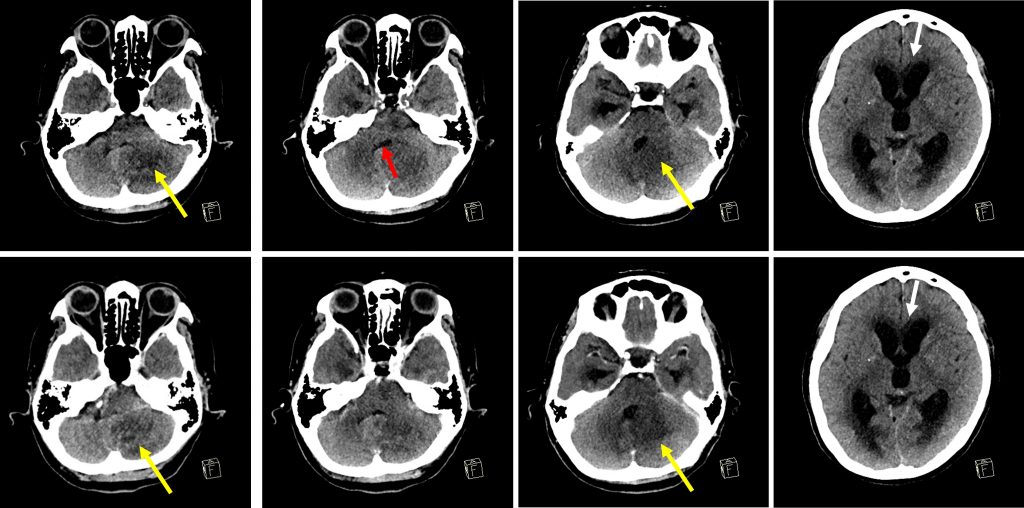
CT scan findings:
- There is an ill-defined hypodensity at the left cerebellum (yellow arrows)
- No enhancement seen post contrast
- No hyperdense area to suggest acute hemorrhage
- Mass effect with compression and narrowing of the fourth ventricle (red arrow)
- There is obstructive hydrocephalus (white arrows)
- Cerebral oedema is also noted.
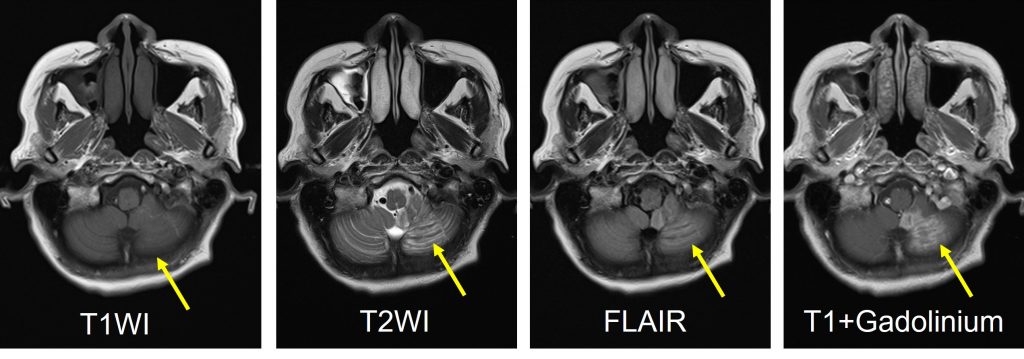
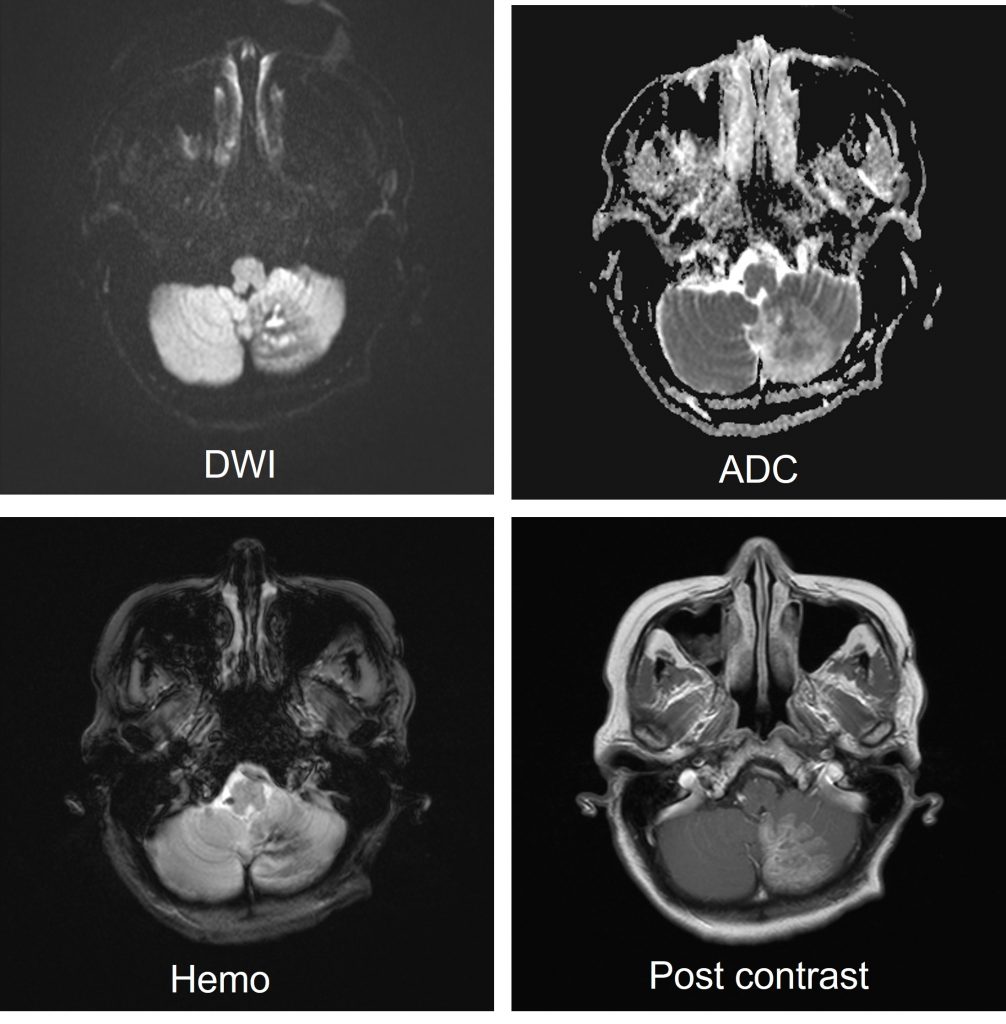
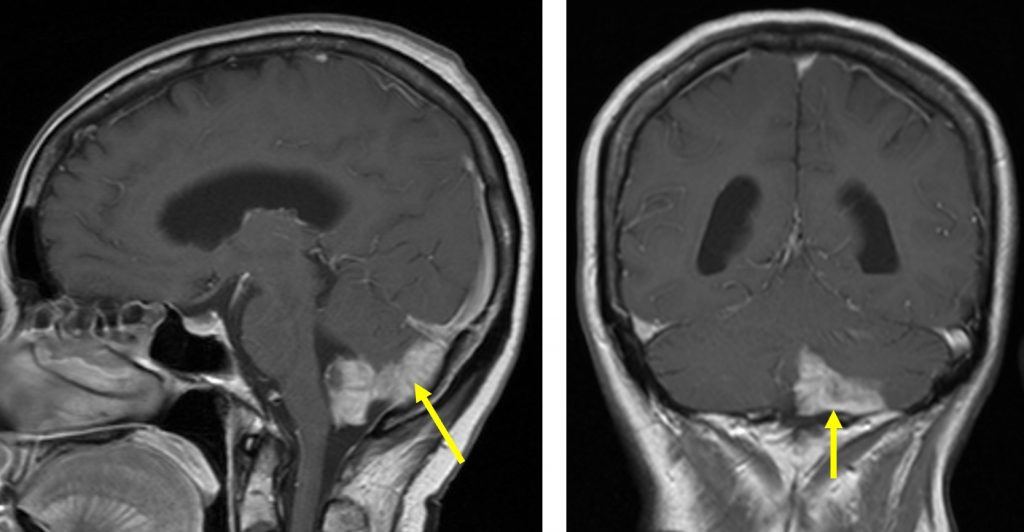
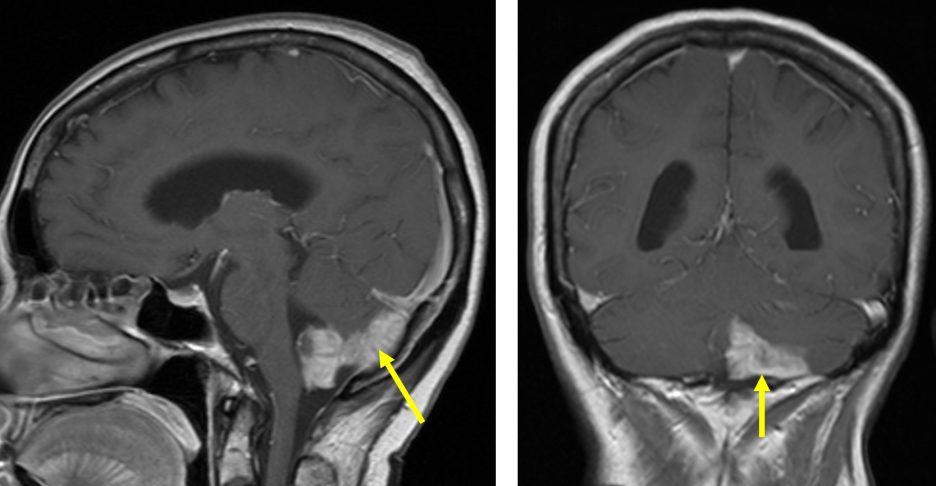
MRI findings (3 weeks after CT scan)
- A T2/FLAIR hyperintensity seen in the left cerebellum
- Post contrast study shows gyriform enhancement at posterior and medial part of left cerebellum which shows territorial distribution
- Areas of restricted diffusion seen within the same region
- No mass effect. No surrounding oedema.
Diagnosis : PICA (posterior inferior cerebellar artery) infarction
Discussion:
- Cerebellar infarction is a relatively uncommon subtype of ischaemic stroke
- It accounts for about 2% of all cerebral infarctions
- On acute stage it is seen as hyperintense area on DWI
- Cerebral oedema peaks about 3 days
- Parenchymal contrast enhancement may be visible 2-4 months after infarction
- Mortality rate is higher due to concomitant brainstem infarction or compressive hydrocephalus rather than cerebellar infarction itself.
Progress of patient:
- Patient underwent Right EVD insertion. Post operative, patient is able to extubate and GCS was E4V5M6.
- Post operative D5, EVD was removed from patient and patient was discharge from ward with early MRI brain appointment.
- Patient is improving and EVD is able to wean off
Recent Comments