Clinical:
- A 21 years old man
- Strep. viridans endocarditis with aortic regurgitation.
- Presented with acute left MCA infarction
- MRI done for further assessment
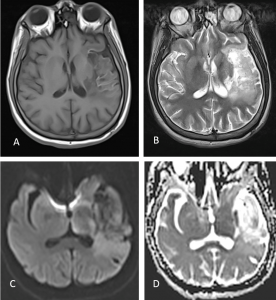
MRI findings:
- MRI done 3 weeks after initial presentation
- There is T1W hypointensity and T2W hyperintense signal in the left MCA territory with associated mild volume loss and cortical laminar necrosis in keeping with subacute infarct.
- There is no evidence of restricted diffusion noted on DWI.
- There are areas of blooming artifact within this region on GRE suggestive of bleed within it (red circle).
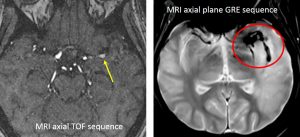
- On TOF sequence, reduced blood vessels at left MCA territory seen (blue circle)
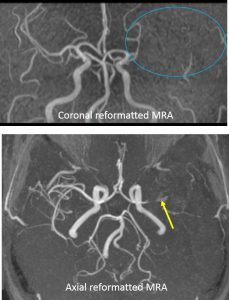
- There is also significant (>70%) stenosis in the M1 segment of the left MCA (yellow arrow). Post stenotic irregular dilatation seen.
- Suspicious aneurysm seen at this post stenotic portion of the artery measuring 3.3 x 4.9 mm
- The overall MRI features are of left subacute MCA territory infarct with haemorrhagic transformation, most probably post infective vasculitis with suspicious aneurysm in the left M1 MCA.
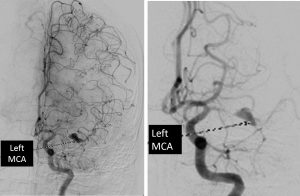
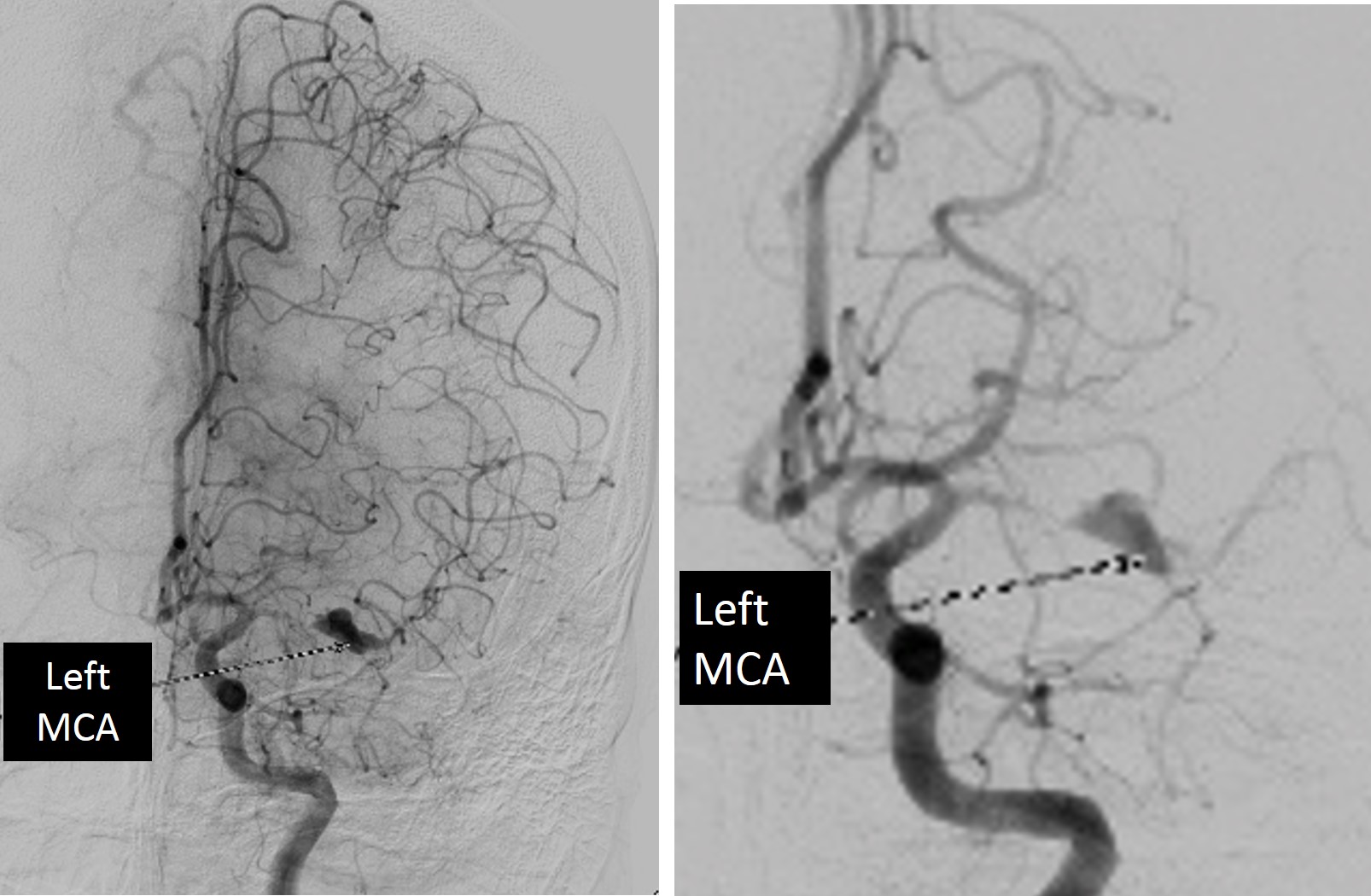
DSA findings:
- There is aneurysm at M1 segment of left MCA measuring about 7x2x3 mm associated with proximal segmental stenosis.
- The M2 segment is relatively normal but the opacification is delayed.
- There is delayed filling of the left M2 branches noted arising from the pial collaterals of ipsilateral ACA.
- PSA run shows no significant collaterals to the left MCA. No AVM.
- Features are consistent with left MCA aneurysm with relatively unremarkable ipsilateral arterial branches likely represent mycotic aneurysm.
Diagnosis: Intracranial mycotic aneurysm
Discussion:
- The prevalence of intracranial mycotic aneurysm is 0.7%-4% among all patients with cerebral aneurysms.
- Infective endocarditis is the primary risk factors of intracranial mycotic aneurysm accounting for about 70% of cases
- In patients with infective endocarditis, up to 5% develop intracranial mycotic aneurysm
- Intracranial mycotic aneurysms are nearly always secondary to bacterial infection. However fungal and viral causes had been reporterd.
- The aneurysm exist due to infection of arterial wall from hematogenous spread (septic emboli).
- Direct extravascular invasion is rare, can be seen in meningitis, thrombophlebitis or orbital cellulitis.
- The infection causes local arteritis resulting in degeneration of the elastic lamina and vessel wall. There is subsequent formation of pseudoaneurysm through hydrostatic pulsations.
- Bacterial intracerebral mycotic aneurysms have predilection for more peripheral points (M2 and beyond) especially the distal middle cerebral artery, compared to berry aneurysm which are generally located at branch points of large circle of willis vessels.
- In direct extravascular invasion, mycotic aneurysms are proximally located.
- Fungal intracerebral mycotic aneurysms tend to involve long segment of large vessels, often not involving branching points at all.
- Aneurysm may be larger and more rapidly growing in immunocompromised patients
- Morphologically, these aneurysms are typically small and fusiform (more common), saccular or sacculofusiform.
- Digital subtraction angiography (DSA) is the gold standard imaging, the most reliable modality for detecting small aneurysms < 3mm in size.
- In 20-33% of aneurysms that are centrally located (proximal to the first bifurcation of the circle of Willis), it can be difficult to differentiate from berry aneurysm. Features that may help to diffentiate include stenosis or occlusion close to the aneurysm, rapid changed in morphology of aneurysm or presence of other aneurysm (mycotic aneurysms tend to be multiple).
Progress of patient:
- Patient was treat conservatively with antibiotics
- Reassessment MRI one and two months later showed reduction in size of previously seen aneurysm with no other complication or new lesion

Acknowledgement:
- Prof. Ahmad Sobri Muda
- Assoc. Prof. Dr Shahizon Azura Mohamed Mukari
- Dr Syazarina Syaris Osman