Clinical:
- A 16 years old boy
- Underlying liver failure
- Presented with poor GCS
- Also had one episode of hypotensive and bradycardia
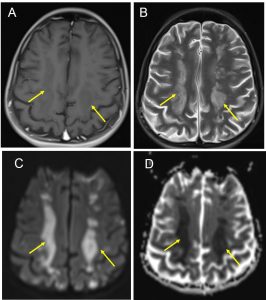
MRI findings:
- Areas of restricted diffusion in white matter at and above level of lateral ventricles, extending from frontal to parietal lobe conforming to anterior and posterior borderzone area
- The changes are hypointense on T1, hyperintense on T2 and FLAIR and show restricted diffusion on DWI sequence
- The changes are bilateral, almost symmetrical with confluent lesions in rosary pattern
- No blooming artifact to suggest bleed
Diagnosis: Acute bilateral borderzone (watershed) infarction.
Discussion:
- Border zone or watershed infarction is also known as hypotensive cerebral infarction
- It is infarction resulting from insufficient cerebral blood flow to meet metabolic demands
- Location: 2 types
- Borderzone between the major arterial territories-typically at gray white matter junction
- Borderzone between perforating arteries-
- Morphology
- Cortical based wedge shaped abnormality between vascular territories
- deep white matter-rosary or string of pearl/beads appearance, multiple round foci in linear orientation within centrum semiovale, can be unilateral
- Pseudolaminar necrosis= curvilinear, gyriform T1-hyperintense regions
- Diffuse supratentorial abnormality following global asphyxia (white cerebellar or reversal sign)