Clinical:
- A 64-year-old man with pituitary macroadenoma.
- Transphenoidal surgery was done 12 years ago.
- He was under yearly MRI surveillance for residual tumour.
- He presented with sudden onset of headache and vomiting.
- Clinical examination showed right temporal hemianopia.
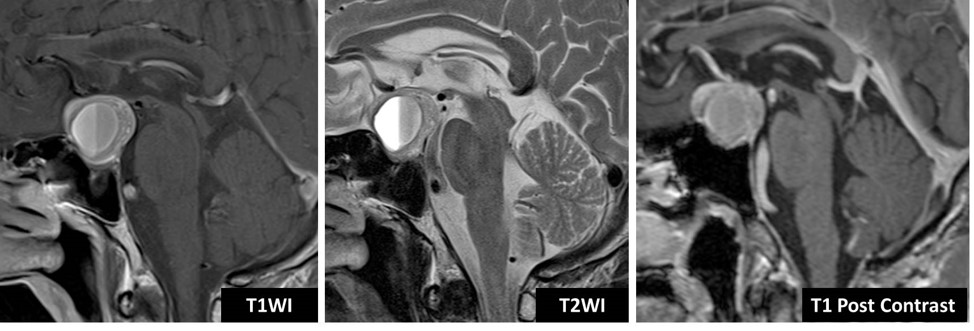
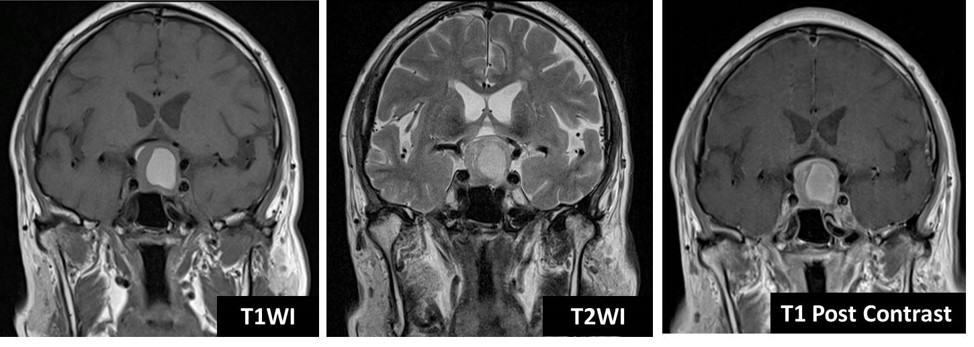
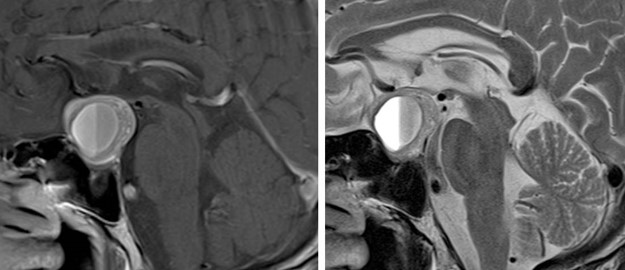
MRI findings:
- There is a sellar mass, larger in size compared to previous MRI (images not shown).
- It is isointense to gray matter on T1WI and T2WI.
- There is a well-defined homogeneous hyperintense change on T1WI, T2WI and not suppressed on fat-suppression sequence (image not shown) suggestive of methemoglobin layering in keeping with subacute intratumoural bleed. Following contrast, the mass enhances heterogeneously.
- Superiorly, the mass bulges upward causing compression unto the optic chiasm.
Diagnosis: Pituitary apoplexy
Discussion:
- Pituitary apoplexy is an acute clinical syndrome caused by either haemorrhage or non-haemorrhagic necrosis of the pituitary gland.
- An existing pituitary macroadenoma is usually present in 60-90% of cases but it can also occur with healthy glands. Additional predisposing factors include pregnancy, trauma and surgery.
- Imaging features include enlargement of the pituitary gland with or without bleed.
- Macroscopic haemorrhage is common and occurs in about 85% of cases.
- CT scan is insensitive to the diagnosis. It may show hyperdense pituitary gland. Fluid/fluid levels may also be evident.
- MRI typically demonstrates a pituitary region mass. T1WI and T2WI appearances are variable depending on blood age and component. Post contrast enhancement is also variable, usually peripheral, but may be difficult to identify due to intrinsic high T1-signal.