Clinical:
- A 41 years old lady
- Presented with gradual abdominal distension
- No altered bowel habit
- Normal menses
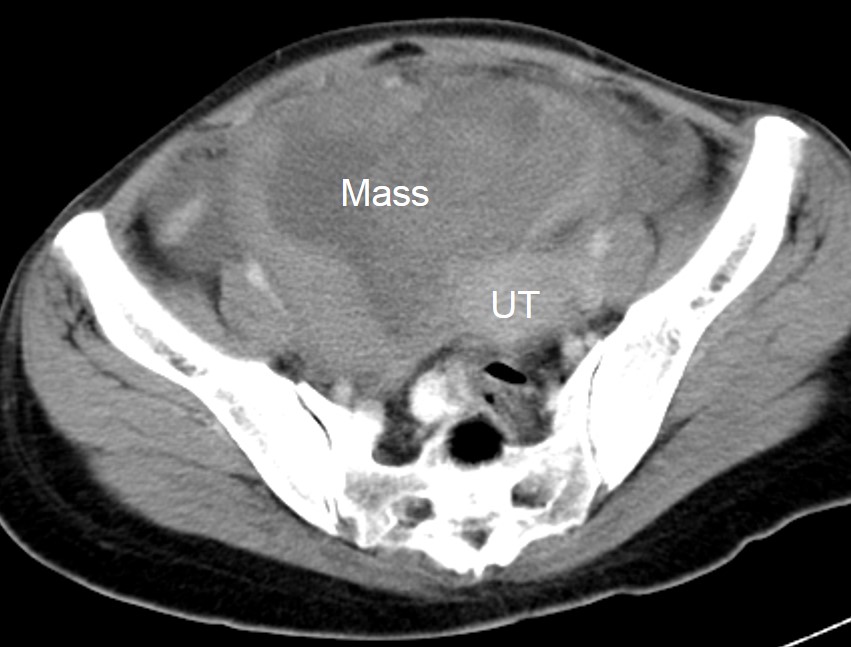
CT scan findings:
- There is a huge abdomino-pelvic mass measuring 13x9x8 cm
- The mass showed mixed density with predominant solid component
- The solid component shows moderate enhancement post contrast
- No calcification or fat component within the mass lesion
- No obvious infiltration into adjacent structures
- Presence of ascites
- Normal ovaries are not identified
Intraoperative findings:
- TAHBSO and omentectomy done
- There are bilateral ovarian tumour
- Left ovarian tumour: 10x10x8 cm, cystic, adherence to left pelvic side wall, descending colon and back of the uterus
- Right ovarian tumour: 8x8x5 cm, cystic as well, adherence to right side wall, bladder, caecum and uterus
- Both lesions ruptured during manipulation extruding fleshy content with pus
- Both fallopian tubes adhered to back of uterus. Hydrosalphinges. The left fallopian tube severed from the uterus proper
- The omentum adhered to both ovaries, uterus and bladder, seem to be studded with tumour nodules, < 5mm in diameter
- Uterus burried within dense adhesions, once released normal size about 6 weeks pregnant uterus
- Bladder pulled up to the fundus of uterus and densely adhered to the antreior part of the uterus. Moderate ascites, blackish in colour and foul smelling
HPE findings:
- Macroscopy: specimen labelled as uterus and adnexa. The right ovarian cyst measures 70x40x30 mm with a wall thickness of 2 to 7 mm. The left ovarian cyst measures 85x65x30 mm with a wall thickness of 2 to 8 mm. Serial cut sections of the uterus shows a small fibroid at the fundus measuring 7 mm in diameter. The uterine cavity and cervical canal are empty. There is a suspicious tumout nodule at the right uterine cornu measuring 7x8x9 mm. The inner surface of both ovarian cysts is covered with brownish material. No solid area seen. The attached right and left fallopian tubes are unremarkable.
- Microscopy: The fibroid and tumour in the uterus are foci of endometrial glands and stroma surrounded by slightly hyperplastic myometrium. Both ovarian cysts are covered in most areas by blood and foamy macrophages. Foci of malignant epithelial lining and glands are seen within the blood on the surface of the cysts. The fallopian tube shows no tumour invasion. There is a foci of endometriosis seen at dilated fallopian tube. There is also haemorrhage on the serosal surface with a few malignant glands within the blood.
- Diagnosis: clear cell carcinoma of both ovaries with endometriosis
Diagnosis: Clear cell carcinoma of ovaries
Discussion:
- Ovarian clear cell carcinoma is quite rare in the western countries but not so uncommon in Asia. The reasons for these differences in incidence around the world and the remarkable difference in incidence among different ethnic populations are not known.
- The mean age of patients is approximately 50 years.
- The risk of this tumour was found significantly elevated in patients with endometrioma of the ovary. The risk increased significantly when the patients were diagnosed at older age, especially over the age of 50, suggesting that the malignant change in endometriosis occurs near menopause.
- It is usually detected at an early stage; 66% of the patients had stage I at the time of diagnosis.
- Treatment strategy for this tumour is basically the same as for other histologic types of epithelial ovarian cancers.
- The tumors were unilateral in majority of cases.
- On CT scan, most of these lesions showed large unilocular cystic masses with solid regions. Most tumors had a well-defined margin. The attenuation of the cystic portion of the mass was relatively high (average, 18 HU). For the cystic portion with attenuation higher than 20 HU, the contents were necrosis or hemorrhage, and for the cystic portion with attenuation lower than 20 HU, the content was serous fluid. This is regarded as a differential point from the other common epithelial origin tumor such as cystadenocarcinoma, because the cystic content of cystadenocarcinoma usually has attenuation similar to that of water.
- For the solid protrusions of the cystic masses, they were relatively small in number. After contrast, the solid components showed heterogeneous enhancements.
- Large peritoneal fluid pockets and peritoneal enhancements are predictive for malignancy