Clinical:
- A 50-year old lady
- She has underlying end stage renal failure and hypertension
- Admitted for dengue fever, complaint of headache
- CT brain on admission was normal
- Clinically there was no bleeding tendency
- Platelet: 18, INR= 3.3, APTT >300.
- Three days later had a fall in bathroom preceded by worsening headache
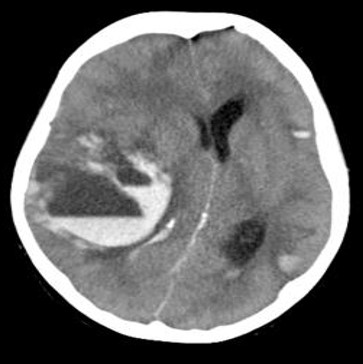
CT scan findings:
- There are multifocal intraparenchymal haemorrhages in both cerebral hemispheres
- The largest are on the right side causing peripheral oedema and midline shift towards the left. There is also mass effect upon the ipsilateral lateral ventricle.
- Many of these hemorrhages demonstrate fluid-blood levels which may be associated with bleeding from a coagulation disorder or anticoagulation.
Radiologic diagnosis: Acute intraparenchymal haemorrhages with blood fluid levels
Discussion:
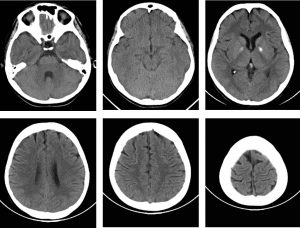
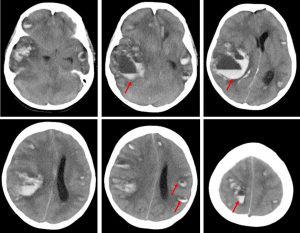
- Fluid-fluid level also described as blood-fluid level or sedimentation level in intracranial haemorrhage can be seen on CT or MRI.
- This is associated with patients who have coagulopathy or who are receiving anticoagulation therapy. These can prevent the formation or lysis of a blood clot, resulting in this appearance.
- On noncontrast head CT, fluid levels within the hematoma are associated with an increased risk of expansion.
- It may rarely be seen in patients with normal coagulation parameters, probably reflecting the fact that the PT/INR does not capture all patients with coagulopathy.
- Higher intensity anticoagulation with increasing PT/INR is associated with a higher likelihood of blood-fluid levels, but many patients with fluid levels may only have mild to moderate PT/INR elevation.
- As the coagulopathy is reversed, the bleeding stabilizes, fluid levels disappear, and the hematoma is eventually resorbed.