Case contribution: Dr Radhiana Hassan
Clinical:
- A 66 years old man
- No known medical illness
- Presented with left ear pain and discharge, associated with high grade fever
- Treated for acute suppurative otitis media and on oral antibiotic for 2 weeks
- Subsequently had abnormal behaviour with slurred speech and right sided hemiparesis
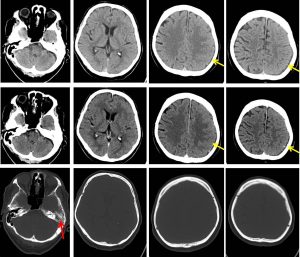
CT scan findings:
- Increased meningeal enhancement at left temporoparietal region (yellow arrow).
- Presence of subdural collection at left parietal region measuring 0.3 cm thickness. There is associated cerebral oedema with effacement of the cerebral sulci on the left side.
- No mass effect or midline shift. No acute intracranial haemorrhage.
- No hydrocephalus. Normal grey white matter differentiation.
- Basal cisterns are not effaced.
- Fluid is noted at left mastoid air cells and left middle ear (red arrow).
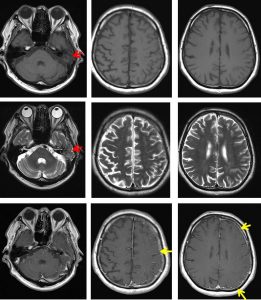
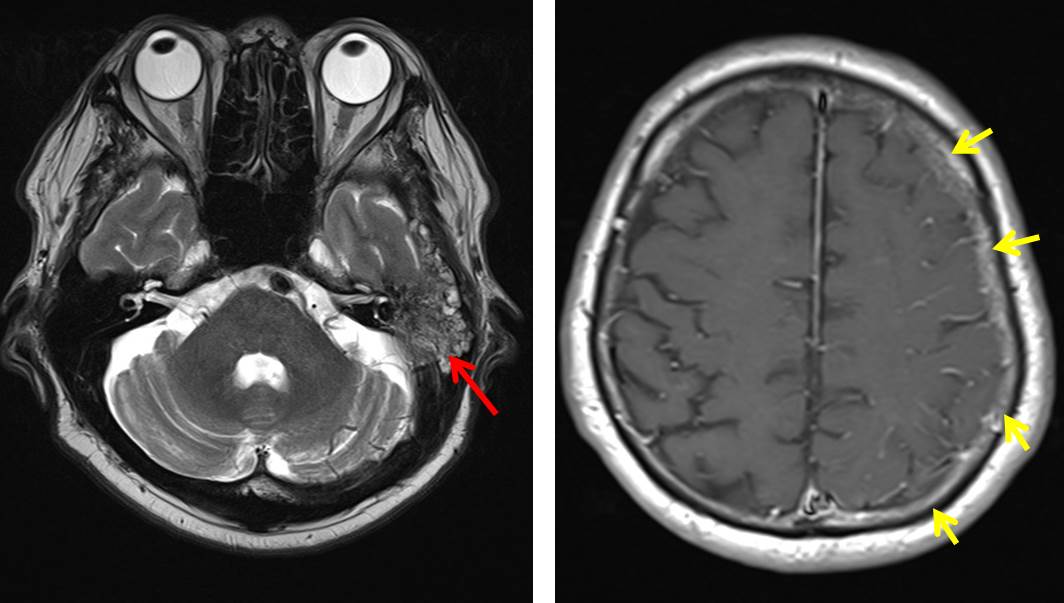
MRI findings:
- Continuous smooth enhancement of the meninges are noted in the left cerebral hemispheres (yellow arrows).
- It is associated with mild effacement of the left cerebral hemisphere sulci and cortical thickening which is mainly seen at left temporo-occipital lobes; suggestive of cortical oedema.
- Grey white matter junction differentiation is however remains preserved. No internal brain herniation.
- No area of restriction diffusion demonstrated in DWI/ADC.
- No blooming artefact seen in hemo sequence to suggest of bleed.
- No enhancing brain lesion is seen.
- The previously seen minimal left subdural collection at left parietal region (at previous CECT) is no longer visualized in this study.
- No hydrocephalus. Basal cisterns are not effaced.
- Left mastoid air cells are filled with fluid signal intensity, suggestive of left mastoiditis.
- Right mastoid air cells are well aerated.
- Mucosal thickening of bilateral maxillary sinuses are noted.
Diagnosis: Left otomastoiditis with meningitis.
Discussion:
- Intra cranial complications from mastoiditis is well recognized.
- Pathways of intracranial spread from infective focus include anatomical contiguity between meninges and mastoid, hematogenous spread, thrombophlebitis of the blood vessel, and bone dehiscence.
- Computed tomography and MRI scan play an important role in diagnosing mastoiditis and its intracranial complications, but sensibility and specificity of these techniques are not definitively established.
- The most common complications in MR imaging were intratemporal abscess, subperiosteal abscess and labyrinth involvement.
- Children had a significantly higher prevalence of total opacification of the tympanic cavity and mastoid air cells, intense intramastoid enhancement, outer cortical bone destruction, subperiosteal abscess and perimastoid meningeal enhancement.
Progress of patient:
- During current admission, patient was newly diagnosed DM and hepatitis B.
- Treated as meningits and mastoiditis with antibiotics.
- Reassessment prior to discharge showed resolved dysphasia with normal neurological examination
- Patient was able to ambulate independently