Case contribution: Dr Radhiana Binti Hassan
Clinical:
- A 62 years old male
- Presented with cough for 3 months
- Associated with pleuritic chest pain and mild SOB
- No night sweat, no fever, no hemoptysis
- Also noted loss of appetite and loss of weight
- Clinically reduced air entry at right lung with crepitations
- Initially treated for recurrent right pleural effusion
- Thoracoscopy and pleural biopsy done

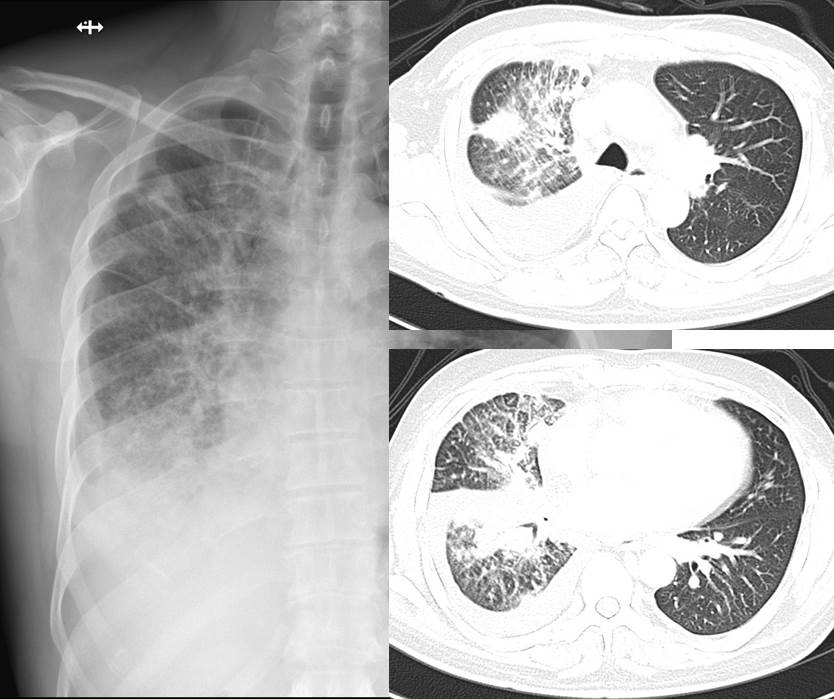
Findings of chest radiograph:
- There is right pleural effusion with obliteration of right hemidiaphragm and meniscus sign
- Patchy air space opacities are seen in the right lung mainly at mid and lower zones.
- No shift of mediastinum, trachea is centrally located.
- No hilar mass.
- No obvious bone abnormality is seen
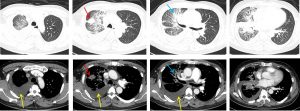
CT scan findings:
- A heterogeneous subsolid lesion with spiculated margins is seen in the right upper lobe (red arrows) which measuring about 2.9 x 2.7 x 3.2cm.
- Consolidations and air bronchogram areas are also seen in the right upper and middle lobe (blue arrows)
- Extensive reticulonodular densities are seen in both right upper and lower lobes, in keeping with lymphangitis carcinomatosis.
- Atelectasis of the basal segments of the right lower lobe is also noted.
- Moderate right pleural effusion noted which is seen tracking into the right oblique fissure.
- Multiple paratracheal and aortopulmonary nodes are seen measuring from 5 mm to 11 mm in sizes.
HPE findings:
- Macroscopy: specimen labelled as right pleural biopsy
- Microscopy: series level show multiple fragments of tissue harbouring malignant cells predominantly arranged as singly dispersed cells. The cells are pleomorphic, having vesicular to hyperchromatic nuclei and some exhibit prominent nucleolus. The nucleoli are eccentric. The cytoplasm is bubbly and vacuolated. There is no glandular formation or squamous differentiation. No epithelioid granuloma is identified.
- Immunohistochemical staining: the nuclei of the tumour cells are positive for TTF-1 antibody.
- Interpretation: Right pleural biopsy: adenocarcinoma.
Diagnosis: Adenocarcinoma of the lung
Discussion:
- Non-small cell lung cancers accounts for about 85% of all lung cancer cases; and of these adenocarcinomas are the most common.
- The peripheral lung adenocarcinoma is previously known as bronchiolo-alveolar carcinoma (BAC)
- It has a wide spectrum of imaging findings from ground glass nodules to solid mass on CT scan.
- The revised classification of terminology from BAC into AIS (adenocarcinoma-in-situ), MIA (minimally invasive adenocarcinoma), LPA (lepidic predominant adenocarcinoma) and predominantly invasive adenocarcinoma reflects better pathologic, radiologic and clinical correlation of this condition.
- However, it is often impossible to radiographically distinguish between these different histological type.
- Solid nodule is defined as a focal area of high attenuation that completely obscures the lung parenchyma and other normal structures within.
- Subsolid nodules is any nodule containing elements of less than solid density. Part solid nodule is a focal opacity containing both solid and ground glass components. Pure ground glass nodule (GGN) are area of high attenuation without obscuration of the underlying lung parenchyma with preservation of bronchial and vascular component.
- The invasive mucinous adenocarcinoma subtype (formerly known mucinous BAC) can have variable appearance including consolidation, air bronchograms, multifocal subsolid nodules or masses.