Case contribution: Dr Radhiana Binti Hassan
Clinical:
- A 12 years old male
- Presented with left knee swelling for 3 years
- Slow growing, associated with on and off pain
- No fever
- Clinical examination shows left knee swelling over posteromedial aspect, hard, non-mobile and non-tender
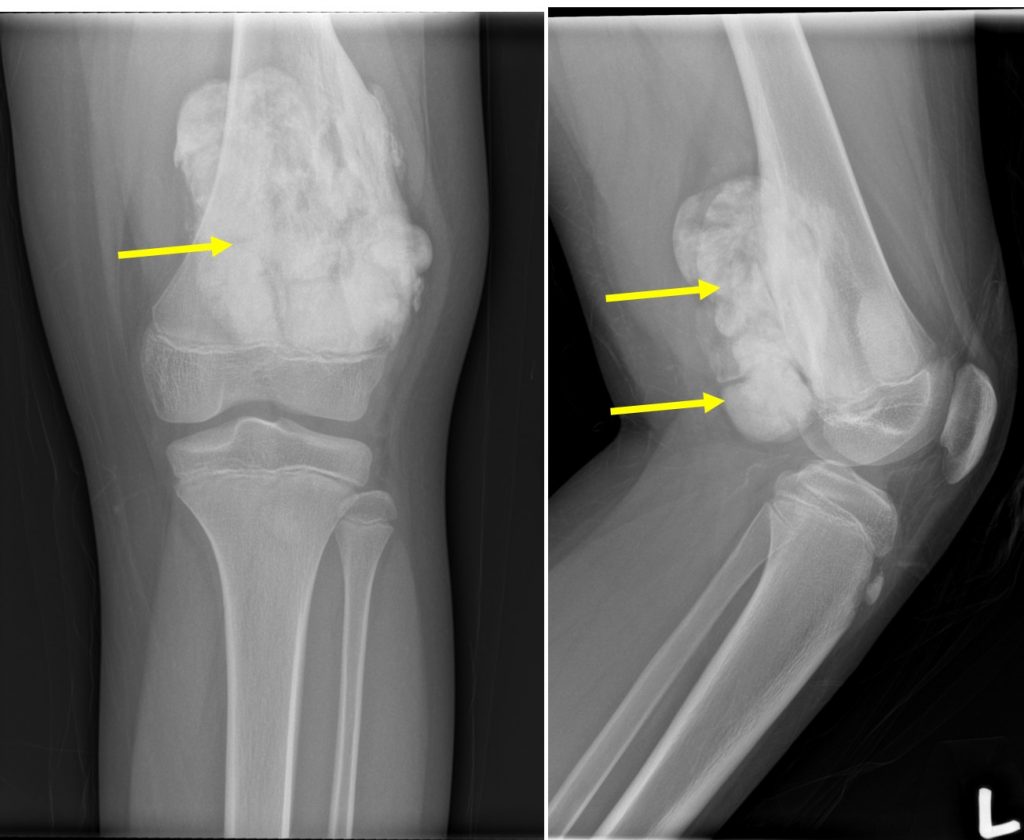
X-ray of right knee in AP and lateral views:
- A large mass at posterolateral aspect of left knee
- Dense opacities of the mass adjacent to distal metaphysis of femur
- It give appearance of cauli-flower and grows away from the femur
- Dense thickening of adjacent cortex is seen
- No aggressive periosteal reaction of the femur
- Thin lucent line is seen between the lesion and posterior cortex of femur
- No extension to epiphysis, no obvious medullary changes
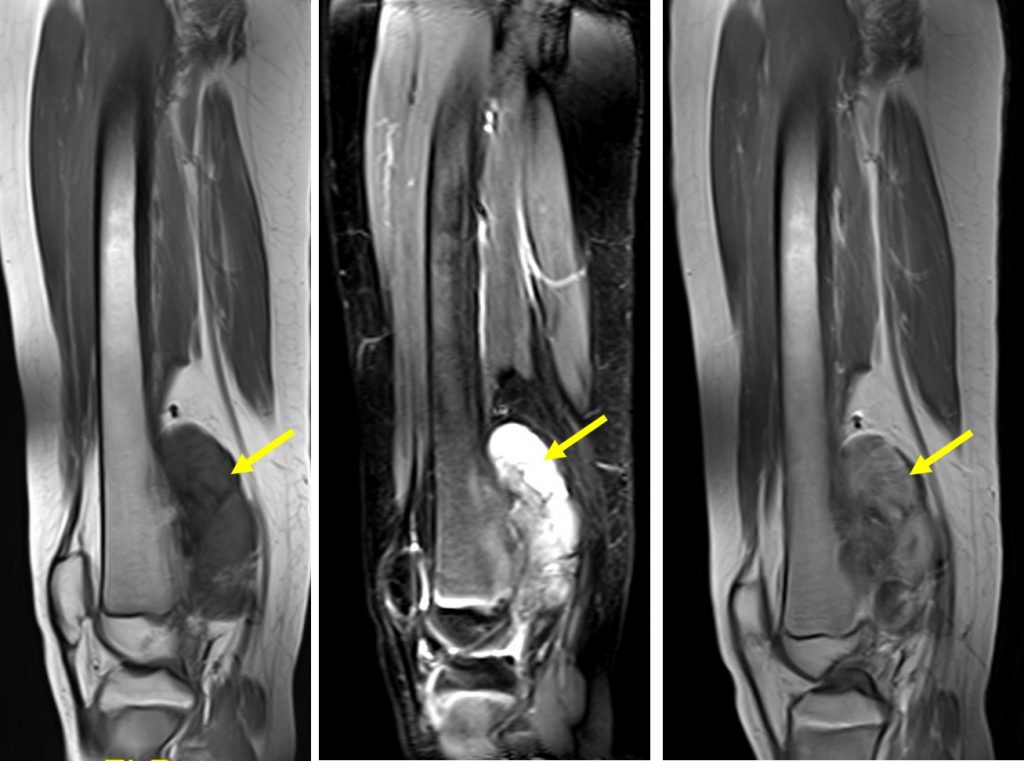
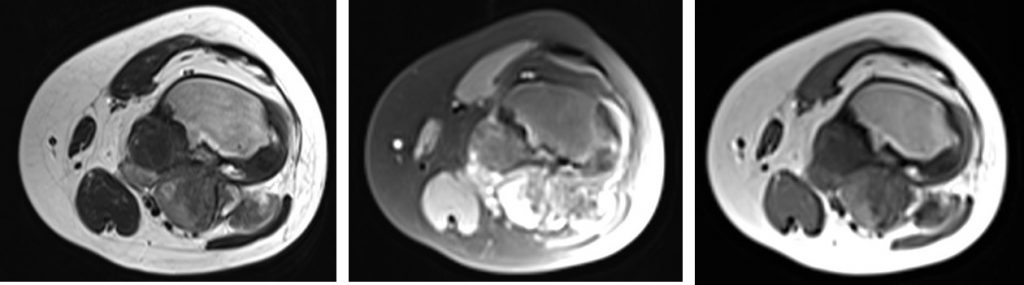
MR findings:
- Lobulated masses protruding from the posteromedial aspect of the metadiaphyseal region of the left distal femur
- Most parts of this masses show thin dark rim in keeping with cortical bone and is consistent with the lobulated bony masses seen on the plain radiographs.
- It shows heterogenous signal on both T1 and T2 weighted, and is not fat suppressed.
- Heterogenous enhancement is seen post IV gadolinium.
- Cortical disruption with scalloping of the posteromedial aspect of the distal femur is seen and 2 well defined rounded cystic lesions which probably contained thick proteinaceous content are seen adjacent to this cortical disruption.
- No abnormal marrow signal is seen in the left femur.
- The adjacent growth plate and knee joint are intact.
- The surrounding muscles are displaced but no abnormal signal intensity is detected within these muscles.
HPE findings:
- Macroscopy: specimen labelled as bone from distal left femur consists of multiple pieces of bony tissue.
- Microscopy: serial and deeper sections shows fibrous and osseous component in varying proportion. The fibrous component composed of principally of bland fibroblastic cells. No mitosis noted. The osseous component is comprised of irregular, trabeculae of woven bone with occasional osteoblasts see. No osteoid production present in this biopsy. No necrosis identified.
- Interpretation: Deeper and serial microscopic examination revealed a lesion consisting of fibrous and osseous component. In view of clinical features and radiological findings, low grade osteosarcoma cannot be excluded.
Diagnosis: Parosteal osteosarcoma
Discussion:
- It is the most common type of juxtacortical or surface osteosarcoma
- It comprises 5% of all osteosarcomas
- Usually presents in early adulthood and middle age
- There is slight female preponderance
- Usually located at metaphysis 80-90%, most common at posterior aspect ofdistal femur (60%) followed by either tibia and then proximal humerus
- Diagnosis is based on a combination of typical histological and radiographic features
- Diagnostic criteria
- Imaging features of a bone tumour
- Parosteal location with origin on the cortical surface of the bone
- Histology of low grade spindle cell tumour with woven bone formation.
- Radiograph
- Large lobulated exophytic, cauliflower like mass with central dense ossification adjacent to the bone
- Tumour periphery less dense than center
- Homogenous ossific mass extending away from cortex
- String sign-a thin radiolucent line separating the tumour from the cortex, seen in 30% of cases
- Tumour stalk-grows within the tumour in late stages and obliterates the radiolucent cleavafe plane
- Cortical thinning without aggressive periosteal reaction is often seen
- Tumour extension into medullary cavity is frequently seen
