Case contribution: Dr Radhiana Hassan
Clinical:
- A 55 years old female with underlying hypertension and diabetes mellitus
- Initially diagnosed and treated as acute rhinosinusitis. Presented with headache and facial pain. Associated with nose discharge and nose block
- Symptoms not resolved after completed antibiotic
- Rigid nasoendoscopy shows thick mucus at right nostril and oedema at OMC. No polyp. FOR normal bilaterally.
- Then noted weakness at opening right eye with progressive blindness.
- Also had generalized body weakness but amble to ambulate independently

X-ray findings:
- Asymmetrical opacity of frontal sinus
- Opacity overlying ethmoidal sinuses region
- Nasal septum centrally located
- Both maxillary sinuses are symmetrical
- No obvious enlargement of the turbinates
- No fluid levels
- No obvious sclerotic or lytic bone changes
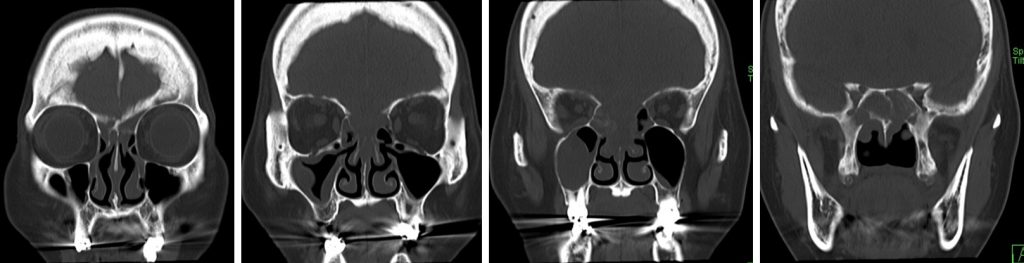
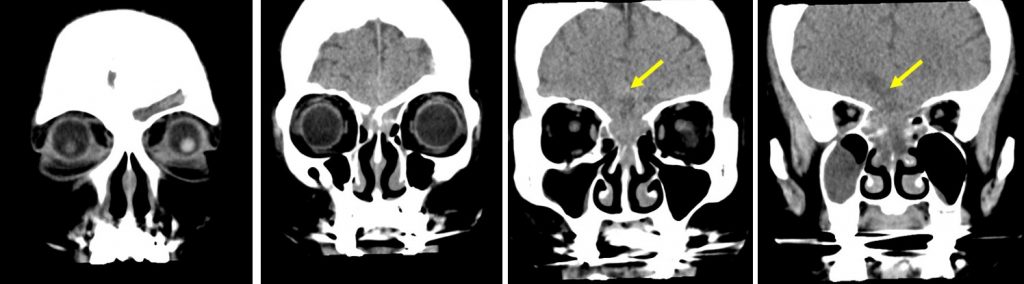
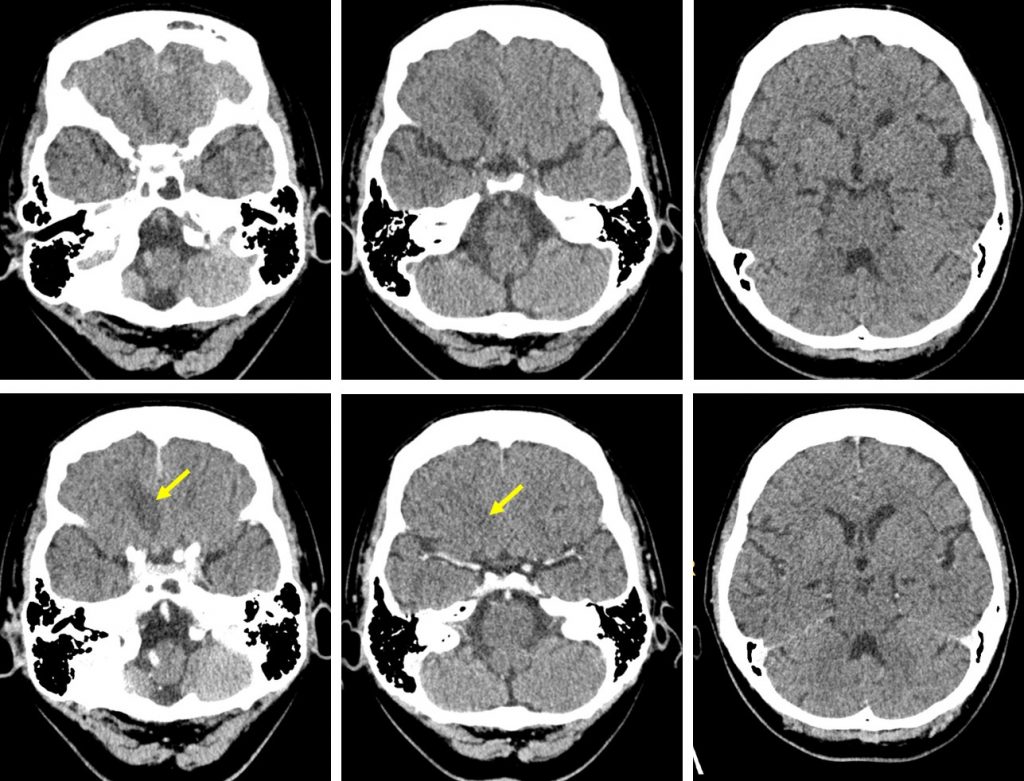
CT scan findings:
- A loculated collection with peripheral enhancement is seen extending from the superior nasal meati bilaterally to the floor of the anterior cranial fossa (yellow arrows). Continuity of the intra- and extracranial components of the collection is observed.
- The intracranial component of the collection measures at 2.1 x 1.7 x 1.5cm (AP x W x CC).
- This is associated with a focal hypodense area seen involving the anterior right frontal lobe, probably representing an area of cerebritis or oedema.
- The intra-nasal component of the collection is seen predominantly on the left superior nasal meatus, with a small right sided component detected. Marked enhancing mucosal thickening is observed intervening in between the loculated collections within the superior nasal meati.
- Erosion of the floor of the anterior cranial is seen at the midline. The superior nasal conchae are largely eroded. There is also erosion of the walls of most of the ethmoidal sinuses.
- Fluid is seen within the sphenoid sinus. Mucosal thickening is also seen within both maxillary sinuses, worse on the right.
- The antra of both ostiomeatal complexes are patent.
- No filling defect seen within the adjacent cavernous sinuses to suggest presence of thrombosis.
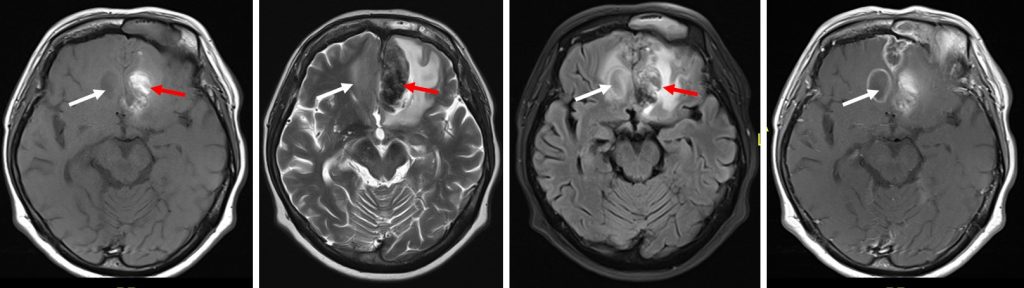
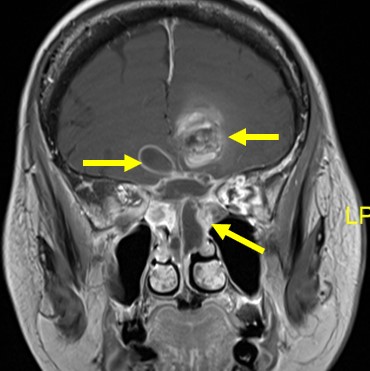
MRI findings:
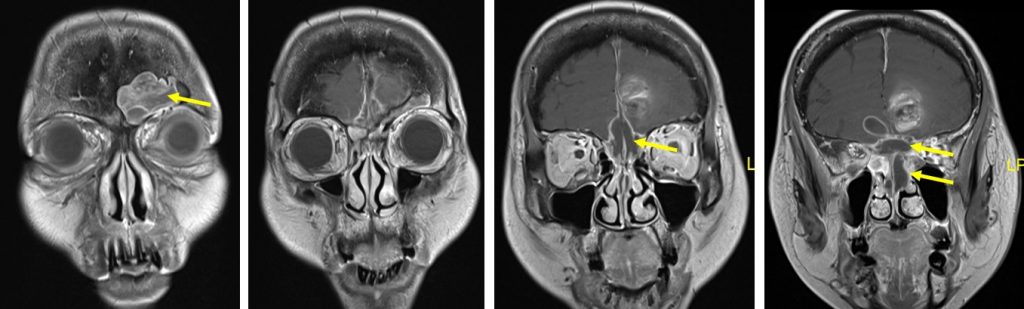
- As seen in the CT scan, a loculated collection with peripheral enhancement is seen extending from the superior nasal meati and ethmoid sinus bilaterally and continuous into the floor of the anterior cranial fossa.
- Anteriorly, the collection is seen extending into the frontal sinus whereby there is a small defect seen in the signal void calvarium with continuity of the peripheral contrast enhancement.
- Posterior extension of the collection is seen occupying the whole sphenoid sinus.
- The cavernous sinus is normal in configuration with no obvious filling defect seen within.
- No significant intraconal extension is observed.
- Both maxillary sinuses are still aerated, with mucosal thickening observed, worse on the right side.
- Bilateral inferior turbinates hypertrophy; more on the left side.
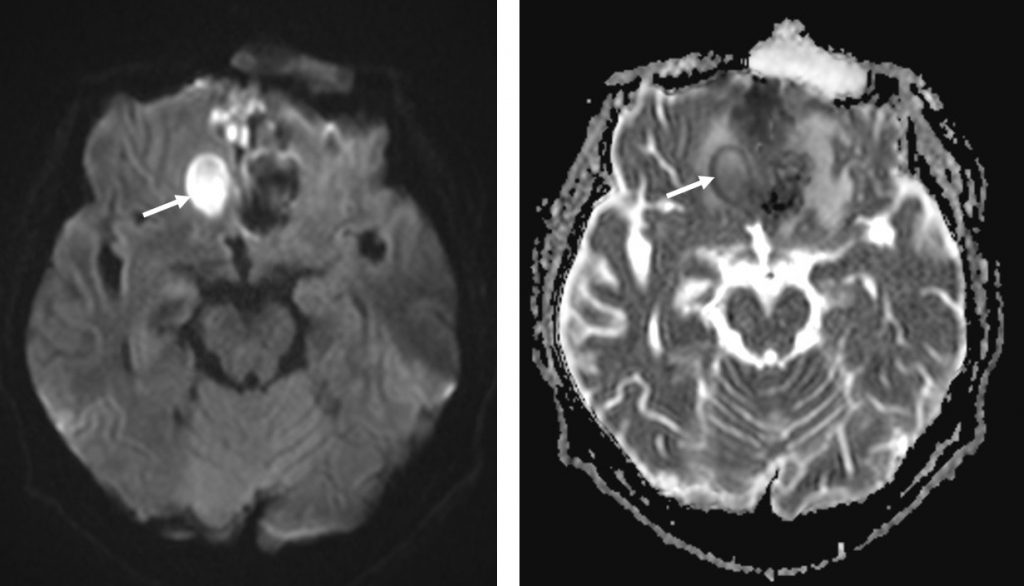
- A well-defined focal intraparenchymal lesion is noted at the right frontal region with minimal vasogenic oedema (white arrows), the lesion appears hypointense on T1, hyperintense on T2 with mild suppression on fluid-suppression sequence. Thin peripheral rim of contrast enhancement is also observed post IV Gadolinium. The lesion also demonstrates restricted diffusion on DWI/ADC. This is suggestive of a focal intraparenchymal abscess.
- A new heterogeneous left parasagittal intraaxial lesion with associated vasogenic oedema and subfalcine herniation is identified at the left frontal region which appears heterogenously hyperintense on T1, hypointense on T2 and T2Flair. Blooming artefact on GRE sequence is also evident indicating hemosiderin deposition but no restricted diffusion or contrast enhancement is observed. This likely represents a focal early subacute intraparenchymal haemorrhage.
- Cerebral venous sinuses appear normal with no filling defect to suggest thrombosis.
Intra-operative findings:
- Bilateral endoscopic sinus surgery and orbital decompression for invasive sinusitis complicated with right orbital apex syndrome and cerebral abscess
- Left ethmoid and maxillary sinuses filled with necrotic mucosa, fluid and pus
- Lamina papyracea appeared brittle
- Sphenoid sinus filled with polypoidal mucosa and pus
- Right ethmoidal sinus filled with necrotic mucosa and pus
HPE findings:
- Macroscopy: specimen labelled as right maxillary sinus tissue and nasal septum tissue
- Microscopy: sections show fragments of necrotic fibrocollagenous tissue with areas of hemorrhage and adjacent granulation tissue reaction. PAS and GMS staining highlight fungal hypae in the nasal septum tissue
- Interpretation: fungal infection
Pus C & S: Aspergillus fumigatus
Diagnosis: Acute invasive fungal sinusitis complicated with cerebral abscess
Progress of patient:
- Multiple surgeries with debridement done
- Completed antibiotics and antifungal
- Recovered but vision remains NPL bilaterally
Discussion:
- Fungal sinusitis is a relatively common misidiagnosed condition involving the paranasal sinuses.
- It is a serious infection associated with a high rate of mortality (50-80%).
- Invasive fungal sinusitis is defined by the presence of fungal hyphae within the mucosa, submucosa, bone or blood vessels of the paranasal sinuses.
- Conversely, non-invasive fungal sinusitis is defined by abscence of hyphae within the mucosa and other tissues or paranasal sinuses
- Acute invasive fungal sinusitis is seen predominantly in immunocompromised patients or patients with poorly controlled diabetes mellitus.
- Clinically it is characterised by painless necrotic nasal septal ulcer, sinusitis, and rapid orbital and intracranial spread.
- Noncontrast CT shows hypodense mucosal thickening or an area of soft tissue within the lumen of involved paranasal sinuses and nasal cavity.
- There is predilection of unilateral involvement of ethmoid and ethmoid sinuses.
- Aggressive bone destruction of sinus wall with intracranial or intraorbital extension of the inflammation.
- These fungi tend to extend along the vessels thus, extension beyond the sinuses can occur without bony wall destruction.
- Intracranial extension leads to cavernous sinus thrombosis, carotid artery invasion, occlusion or pseudoaneurysm with resultant infarction or hemorrhage.
- MRI is superior to CT scan in demonstrating intracranial and intraorbita extension.
- Initial findings include cerebritis, leptomeningeal enhancement and inflammation of the orbital fat and extraocular muscles
- More progressive infection causes granulomas, cerebral abscess and infarctions.